A small compilation of nurse anesthesia care plans
These anesthesia care plans are meant to inspire nurse anesthesia residents when they are making their care plans. Always make sure you fully understand and "own" your care plan. Your plan must be specific for your patient and should always be with the most up-to-date information.
Aortic Stenosis
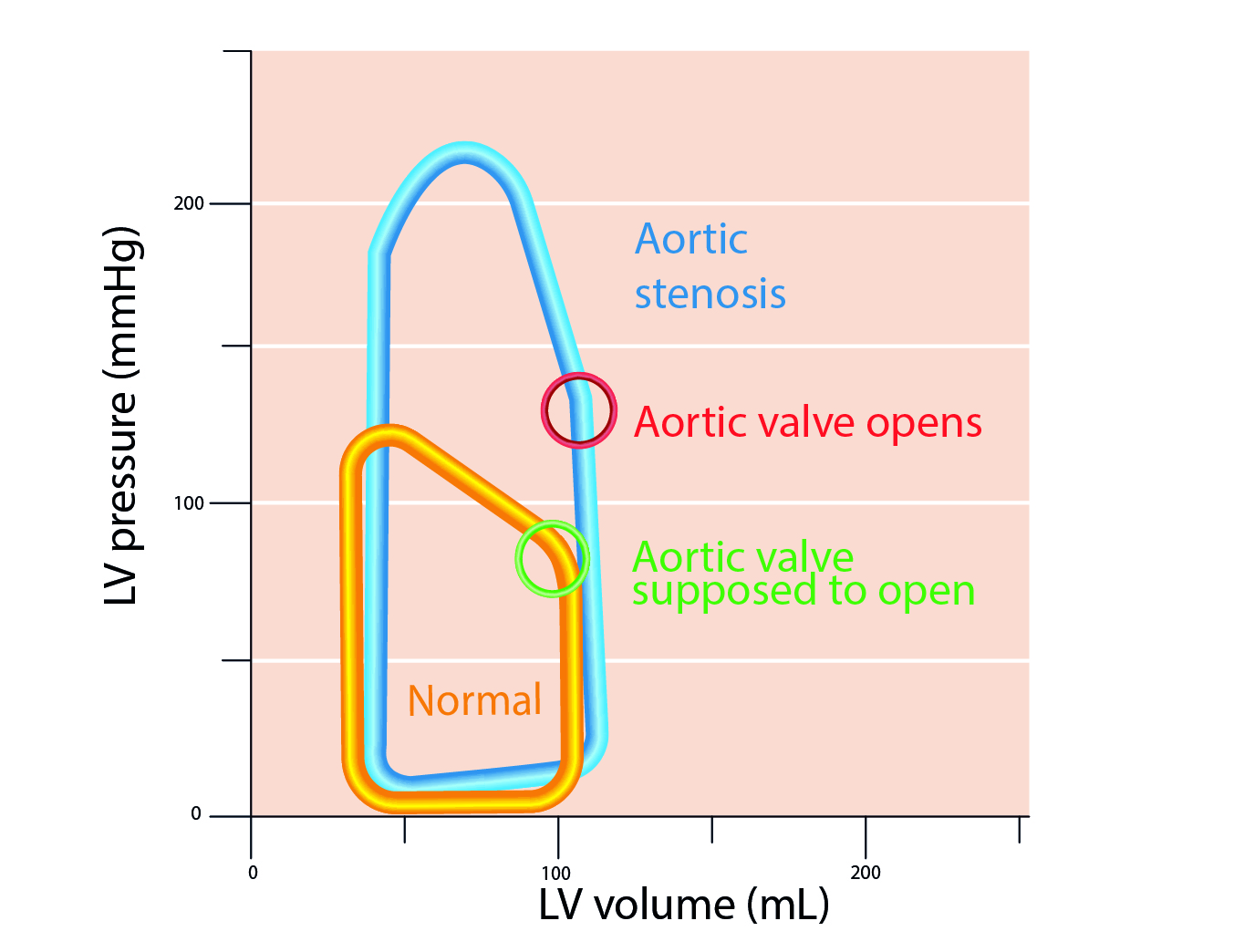 Problem: In Systole (cannot eject)
Problem: In Systole (cannot eject)
Physiologic Considerations
LV preload
Increase or maintain, maintain stroke volume (SV), avoid venodilation – maintain SVR
HR - 70-90
Extremes are not tolerated well. A-fib causes loss of atrial kick. Bradycardia will decrease CO due to fixed SV. Tachycardia will cause decreased CPP and ischemia
Contractility
Maintain constant
SVR
Normal to high. Afterload is a stenotic valve. Increased SVR = Increased LVEDP and/or LVEDV = Increased MVO2
PVR
Maintain constant
Aortic Valve Anatomy
3 leaflets
2.5-3.5 cm2
Peak gradient <10 mmHg
Aortic Stenosis
- Normal: 2.6-3.5 cm2
- Mild: valve area > 1.5 cm2 = Asymptomatic
- Moderate: valve area = 0.7-1.2 cm2
- Severe: valve area <0.7 cm2, gradient >50 mmHg
Etiology
- Congenital bicuspid (40-60 yr)
- Degenerative calcification >70 yr
Symptoms
Angina - 5 yr survival
Syncope - hypoperfusion
Dyspnea/CHF - 2 yr survival
A-fib
Narrow pulse pressure <50
Surgery
NYHA class III and IV
Valve area < 0.9 cm2, LV hypertrophic
Aortic valve gradient > 50mmHg
Cardiac Remodeling
§ LV concentric hypertrophy
§ Increased LVEDP, LVEDV, LAP > 25-30 mmHg
§ Increased LA contribution to LV filling
§ Increased MVO2
§ Decreased O2 delivery = ischemia
§ Pulmonary HTN
§ RV failure
Preop Considerations
§ Angina, syncope, dyspnea
§ Systolic ejection click, holosystolic harsh murmur radiation to carotids. Diminished carotid pulses
§ EKG
§ LVH
§ AV- conduction blocks
§ ECHO to determine the size, severity, and pulmonary HTN
TEE
Measure gradient
Calculate valve area/valve morphology
Perioperative
Light premeds
Monitor hemodynamics
Prophylactic antibiotics (teeth/ infection)
GA- Regional (HOTN)
Phenylephrine gtt mixed
Surgical Technique
Myocardial protection difficult
Hypertrophied ventricle – cardioplegia ante grade / or retrograde via LV vent (via pulmonary veins as aorta open)
Cardiopulmonary bypass temperature 25-28 degrees C
Post Bypass
Maintain preload
SR - avoid tachycardia/bradycardia
Inotropic support (inadequate protection leads to poor revascularization)
Avoid increased afterload
Mechanical vs Tissue Valve
Mechanical
- Longer life, requires anticoagulation
Tissue
- Shorter life expectancy of 10-15 years, minimal to no anticoagulation (ASA)