A small compilation of nurse anesthesia care plans
These anesthesia care plans are meant to inspire nurse anesthesia residents when they are making their care plans. Always make sure you fully understand and "own" your care plan. Your plan must be specific for your patient and should always be with the most up-to-date information.
Axillary block
 Know the landmarks, what you go through, what can go wrong, and the treatment and response for any block.
Know the landmarks, what you go through, what can go wrong, and the treatment and response for any block.
Brachial Plexus runs deep to the clavicle and superior to the 1st rib.
Remember, the nerves in the body usually run with vessels, which are used as landmarks.
Axillary Block
The axillary block is used for surgery on the hand and forearm but can also be used for elbow surgeries
Risk of missing the musculocutaneous branch
Any patient who is unable to abduct more than 45 degrees at the shoulder is not an appropriate candidate for the axillary block
The axillary block targets four terminal branches of the brachial plexus
Brachial Plexus
- R - roots
- T - trunks
- D - divisions
- C - cords
- B - branches
The plexus divides into five main terminal branches
- Median nerve - middle finger flexion
- Radial nerve - thumb abduction
- Ulnar nerve -little finger flexion, 4th and 5th finger movement
- Musculocutaneous nerve - need to see biceps movement with blockade
- Axillary – deltoid muscle
Block Placement
Connect the patient to the pulse-ox opposite arm, EKG, and O2 N/C. Perform the BP measurement while the patient is supine, arm flexed 90 degrees, and lying overhead.
Equipment
Gloves, Betadine, towels for some blocks, sterile insulated short bevel needle, nerve stimulator, sedation (Versed and Fentanyl), LA (with epinephrine to evaluate for intravascular injection), local anesthetics for skin, skin marker and ruler, competent assistant
May use Naropin 0.5% - 60 mL = 300 mg. It may last 4-6 hrs, with epi 8-12 hrs.
Max dose 3 mg/kg
Monitor with one EKG pad on the patient from the stimulator. Start with 1.2 mA and go down to 0.5 mA. Ensures appropriate proximity to the nerve. If you are below 0.3 and still get stimulation, you may be intraneural and don't want to inject here
Chart stimulation threshold
Continuous aspiration when the needle in the tissue
Technique
Transarterial
Locate the axillary artery, insert the needle, and aspirate until bright, red blood is obtained
The needle is then advanced or withdrawn until there is no blood aspiration
Usually, inject both posteriorly, anteriorly, or both. 40-60 mL, 1/2 posterior, 1/2 anterior - this varies
Nerve Stimulator
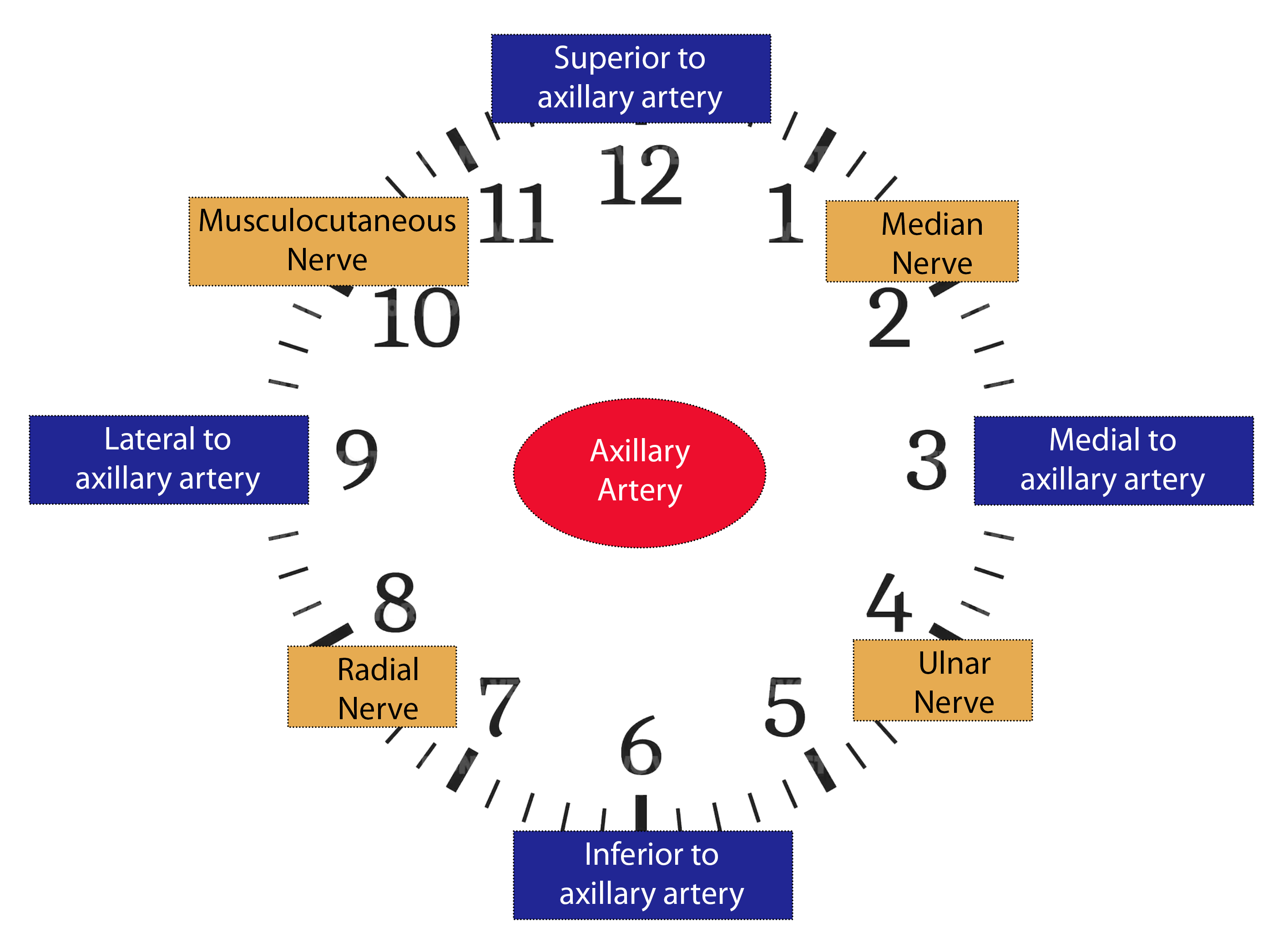
The axillary artery is pinned parallel to the fingers. The median nerve lies superior to the pulse, the ulnar nerve lies inferior, and the radial nerve is inferior/posterior to the pulse. The musculocutaneous nerve is separate and deep within the coracobrachialis muscle, which is superior and at risk of being missed.
Complications
This is rare due to the distance between neuraxial structures and the lung
Systemic toxicity (tingling, perioral numbness, metallic taste)
Postoperative neuropathy