A small compilation of nurse anesthesia care plans
These anesthesia care plans are meant to inspire nurse anesthesia residents when they are making their care plans. Always make sure you fully understand and "own" your care plan. Your plan must be specific for your patient and should always be with the most up-to-date information.
Cystoscopy w/Deflux injection
Vesicoureteral reflux (VUR)
Reflux occurs when urine from the bladder flows back up into the ureter and kidneys due to a problem with the valve mechanism. Pressure from the urine filling the bladder should close the tunnel of the ureter and prevent urine from flowing back into it. However, reflux can occur when the ureter enters the bladder at an unusual angle or when the length of the ureter tunnels through the bladder wall is too short.
Vesicoureteral reflux becomes a problem when the urine in the bladder becomes infected. The infected urine quickly travels backward to the kidney, where it can cause a kidney infection. Kidney infections lead to kidney damage.
Risk factors are female gender, age less than 2 years, and Caucasian race.
Diagnosis
Vesicoureteral Reflux is usually discovered during an evaluation for a urinary tract infection (UTI)
A voiding cystourethrogram (VCUG) is an X-ray test in which a small tube or catheter is placed into the bladder through the opening where the urine comes out. X-ray contrast is used to fill the bladder through the catheter. When the child's bladder is full, the child will urinate into a special container while on the X-ray table. While the bladder is filling and the child is urinating, x-rays are taken.
A nuclear cystogram may be used instead of the VCUG. A catheter is placed, and the procedure is like the above test.
A renal and bladder ultrasound is a test using sound waves to look for kidney scarring and to measure kidney size.
Treatment
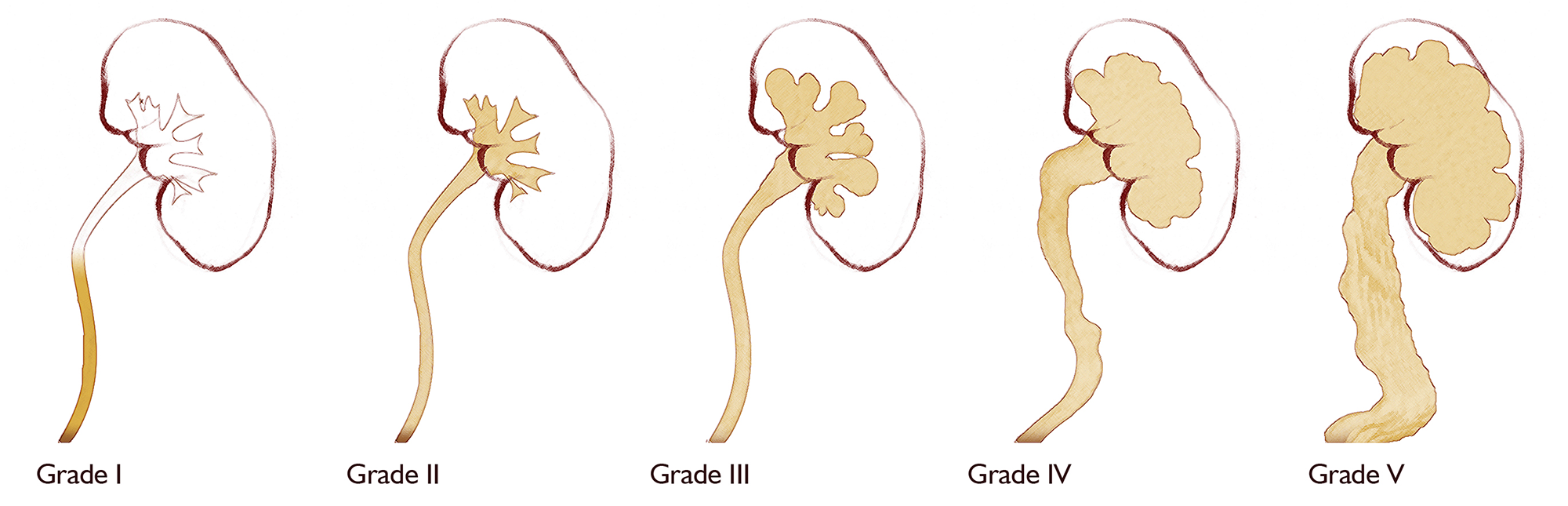 Managing vesicoureteral reflux depends on the grade of reflux, which the VCUG determines. Other factors considered are the frequency of urinary tract infections, the presence and progression of kidney damage, and parental opinion.
Managing vesicoureteral reflux depends on the grade of reflux, which the VCUG determines. Other factors considered are the frequency of urinary tract infections, the presence and progression of kidney damage, and parental opinion.
International Reflux Classification. Adapted from (2002) Vesicoureteral Reflux. In: Belman, King, Kramer (eds.) Clinical Pediatric Urology. London, England: Martin Dunitz, Ltd., 753.
Grades I-III
For grades I-III, there is a good chance that the reflux will disappear as the child grows and the bladder matures. These children are given low-dose antibiotics daily to suppress bacteria from growing. Occasional blood tests and urine cultures may be ordered.
Grades I-IV
An option for patients with grades I-IV is a cystoscopy with a deflux injection. This outpatient procedure involves a small telescope being inserted into the bladder through the urinary opening under general anesthesia. A gel (Deflux) is injected where the ureters enter the bladder. A small bulge is formed in the bladder wall, preventing urine backflow.
Grades IV-V
Patients with "high-grade" reflux, grades IV-V, will take low-dose antibiotics and undergo periodic blood tests, X-ray tests, and urine cultures. These children often need ureteral reimplantation surgery to correct the reflux and prevent progressive damage to the kidneys.
Ureteral Reimplantation Surgery
Surgery aims to correct reflux, prevent pyelonephritis, and preserve renal function. Although the surgical repair of reflux may not stop the development of bladder infections, it will reduce the chance of a bladder infection developing into a kidney infection.
The ureteral reimplantation surgery consists of creating a longer tunnel of the ureter through the bladder wall. The surgery is performed through an incision (cut) just above the pubic bone (bikini incision). If both ureters need to be reimplanted, this is done through one incision.
This surgery usually lasts between 2 ½ and 3 hours. Afterward, the child will be admitted to the hospital for 2-4 days. Before surgery, the anesthesiologist will discuss a pain management plan with the family.
After Surgery
After reflux surgery, there may be limitations on physical activity depending upon your surgeon. Voiding every 2-3 hours, as well as drinking adequate fluids, helps healing. Your child may return to school the day after surgery