A small compilation of nurse anesthesia care plans
These anesthesia care plans are meant to inspire nurse anesthesia residents when they are making their care plans. Always make sure you fully understand and "own" your care plan. Your plan must be specific for your patient and should always be with the most up-to-date information.
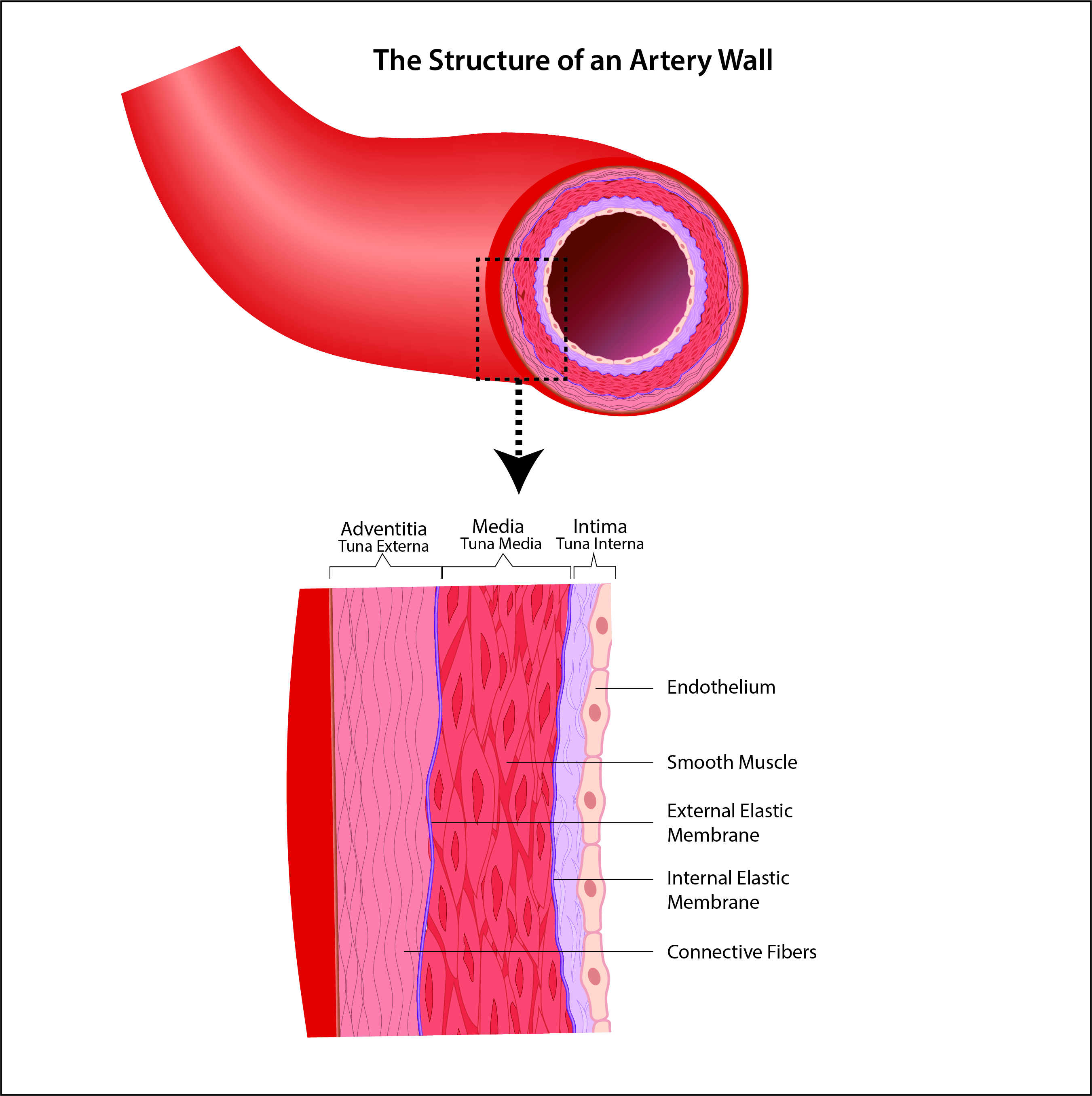
Hemostatic Mechanism
Hemostasis occurs in the blood vessels. The clotting process is triggered by the loss of the endothelial surface
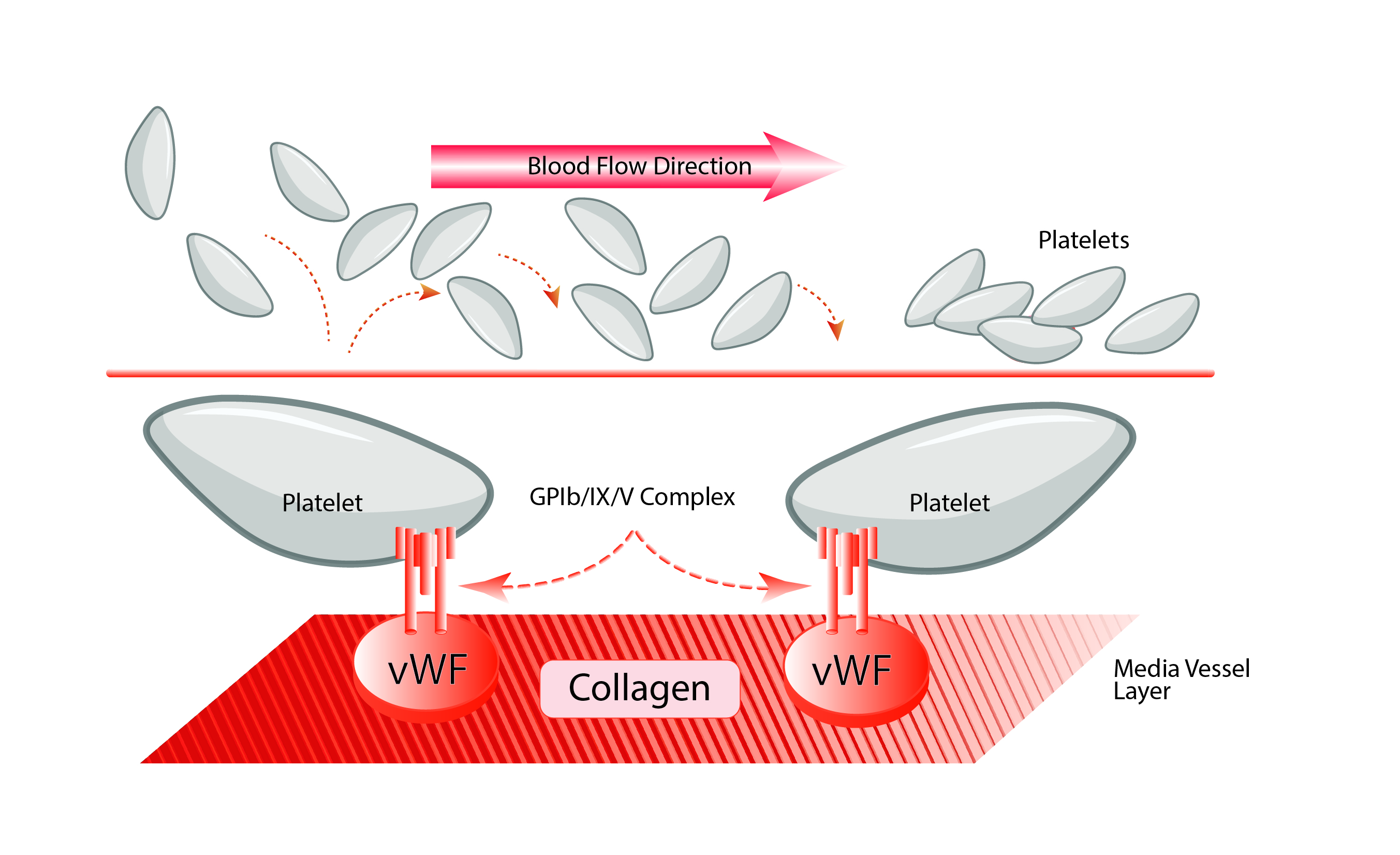
Adhesion
When activated, platelets begin adhering to the collagen layer of the subendothelium via specialized surface receptors.
In venous circulation with low flow conditions, platelets can adhere to surfaces coated with collagen, fibronectin, or laminin.
However, in arteriolar or microcirculation, with high flow conditions and greater shearing forces, platelets are anchored to the subendothelium by von Willebrands factor, blood coagulation factor VIII:vWF.
Platelets Formation
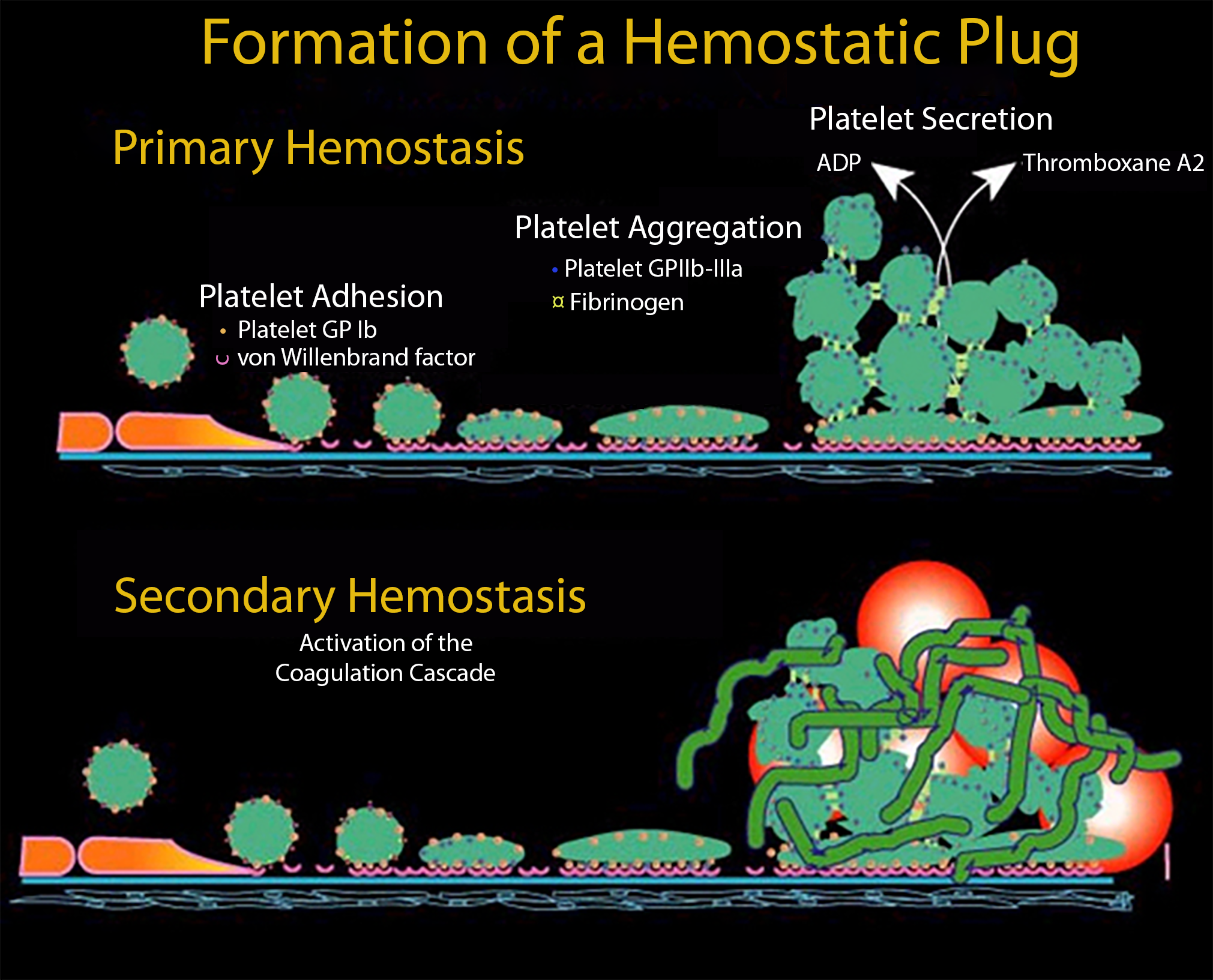
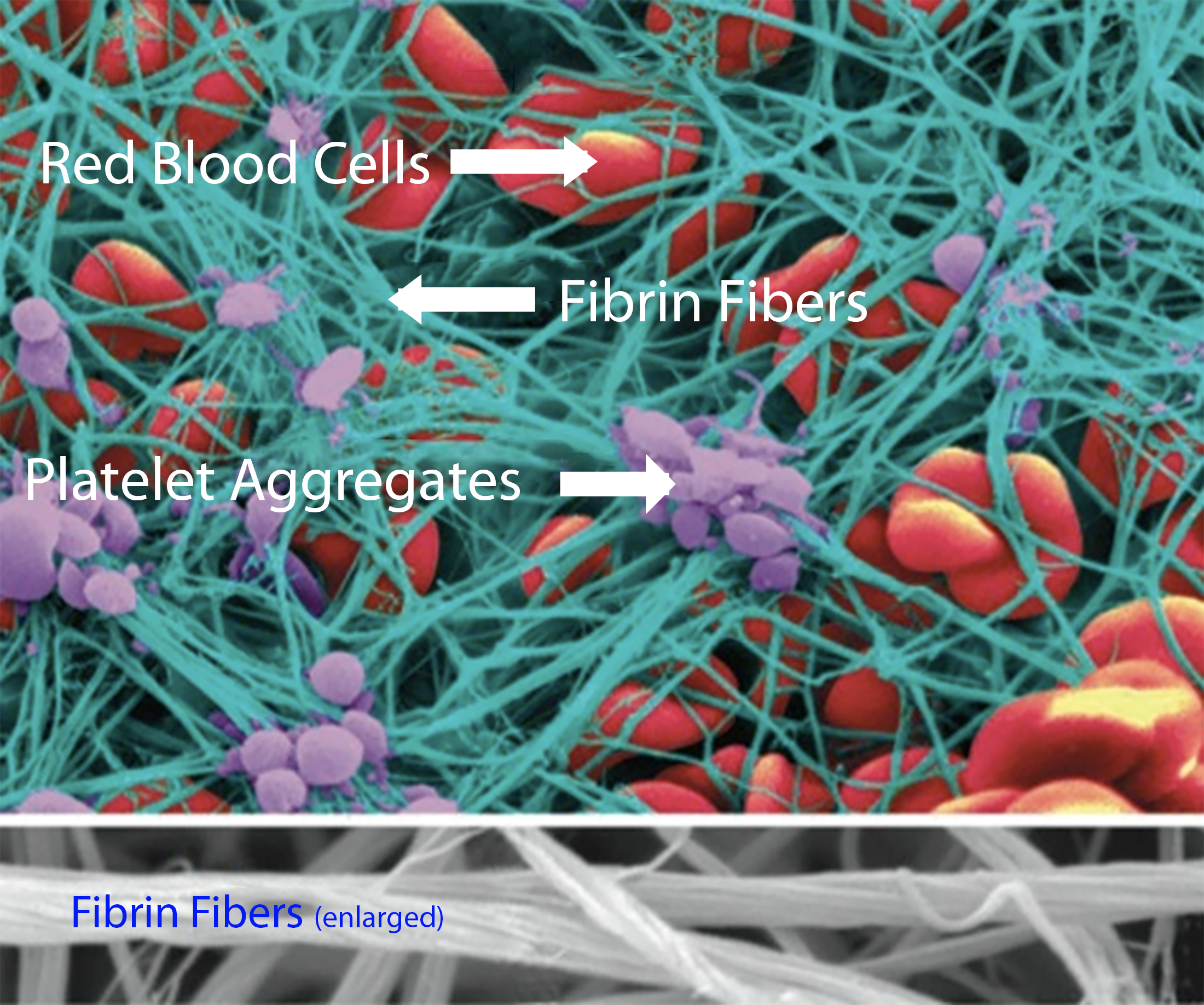
Coagulation involves the interaction of numerous clotting factors in a cascade of events that generate fibrin to reinforce the friable platelet plug.
Secondary Hemostasis
Fibrin is woven and cross-linked among and around red blood cells and aggregated platelets, forming a stable and permanent clot.
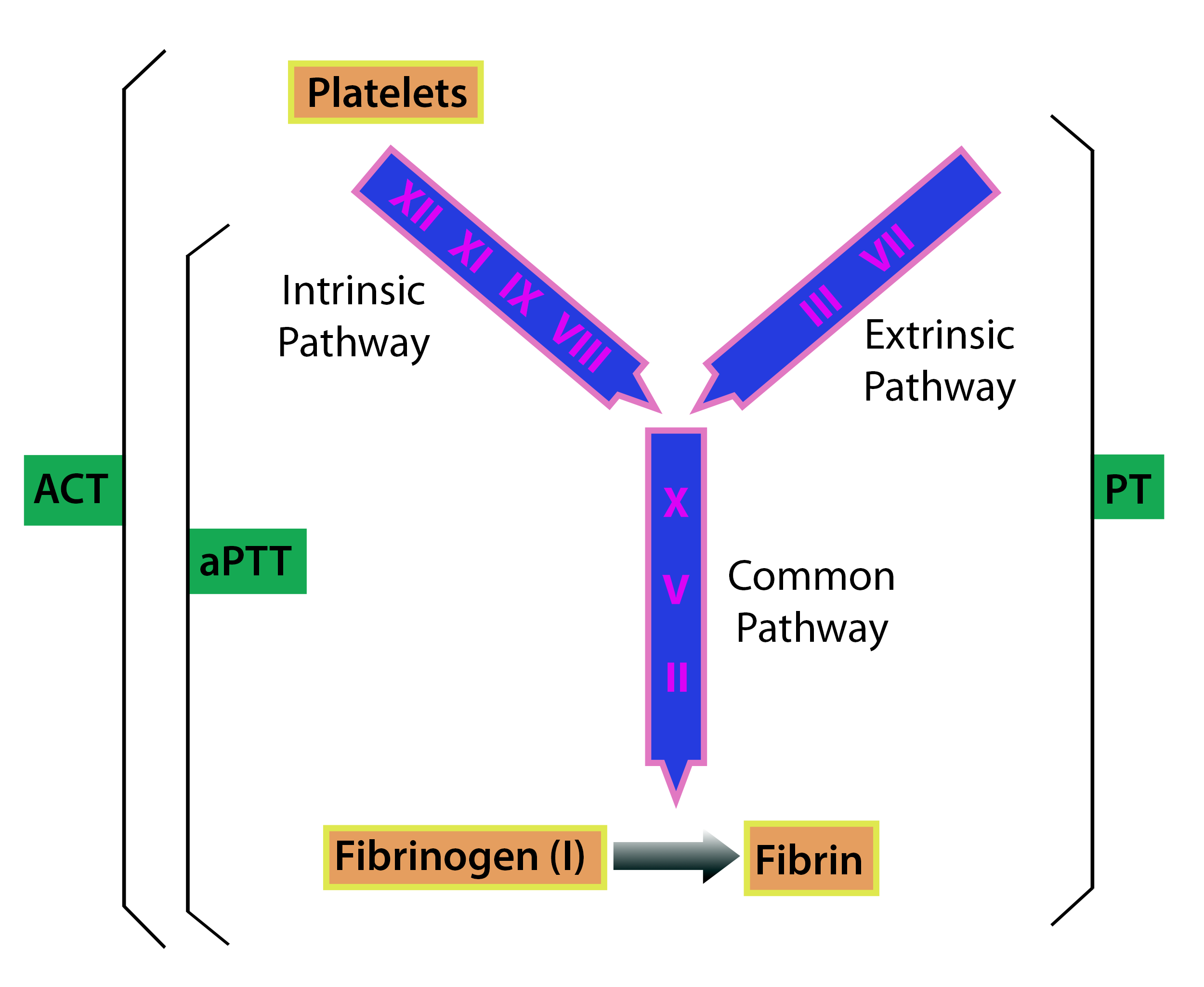
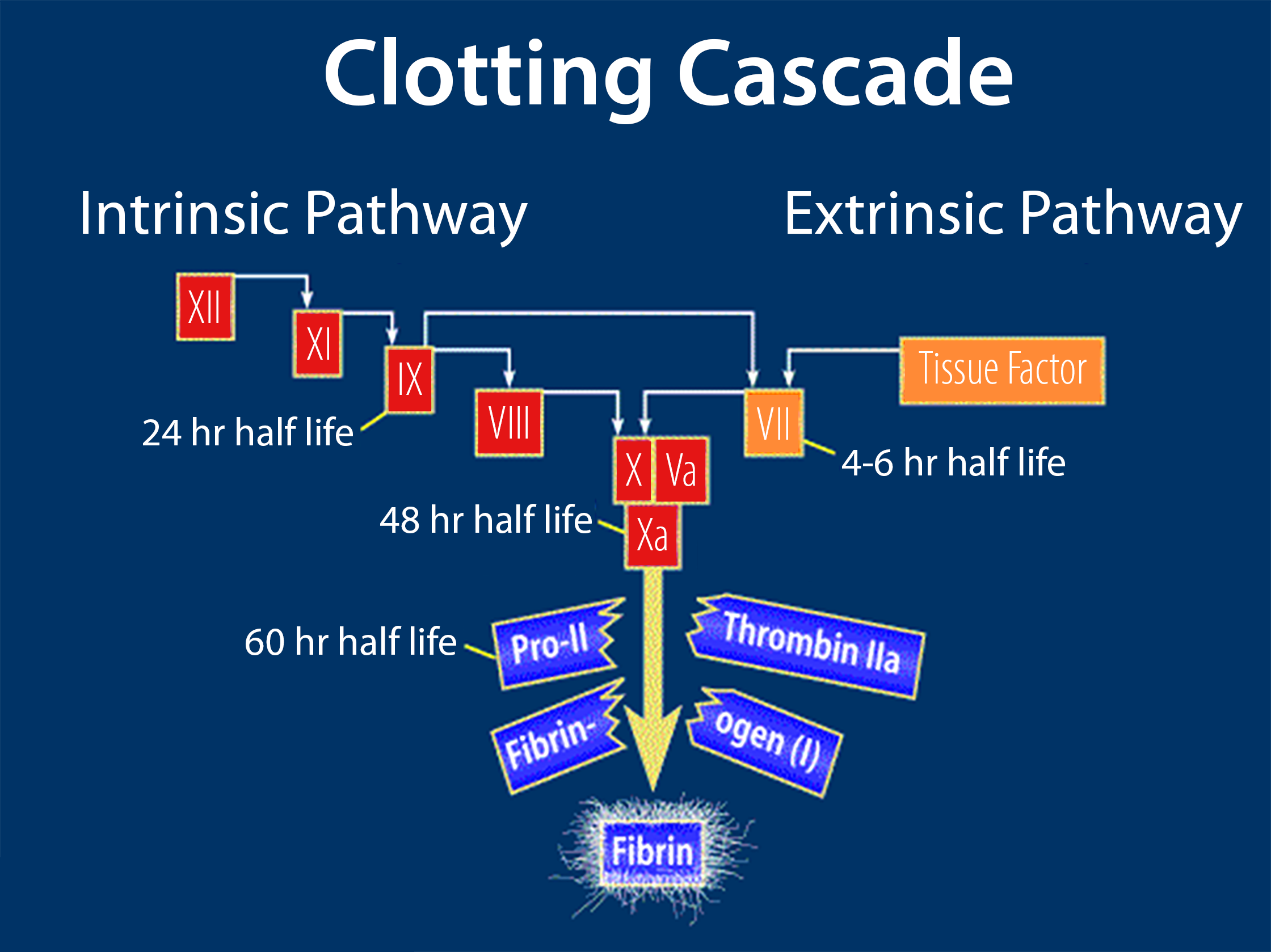
The final steps in fibrin production involve the intrinsic, extrinsic, and final common pathways.
Coagulation Models
An overview for rapid memorization.
Coumadin
Clotting factors (Factors IX, VII, X, and II) are Vitamin K-dependent; therefore, the Vitamin K antagonist warfarin decreases their activity.
Factor VII has the shortest half-life of the Vitamin K-dependent coagulation factors.
Blood component therapy
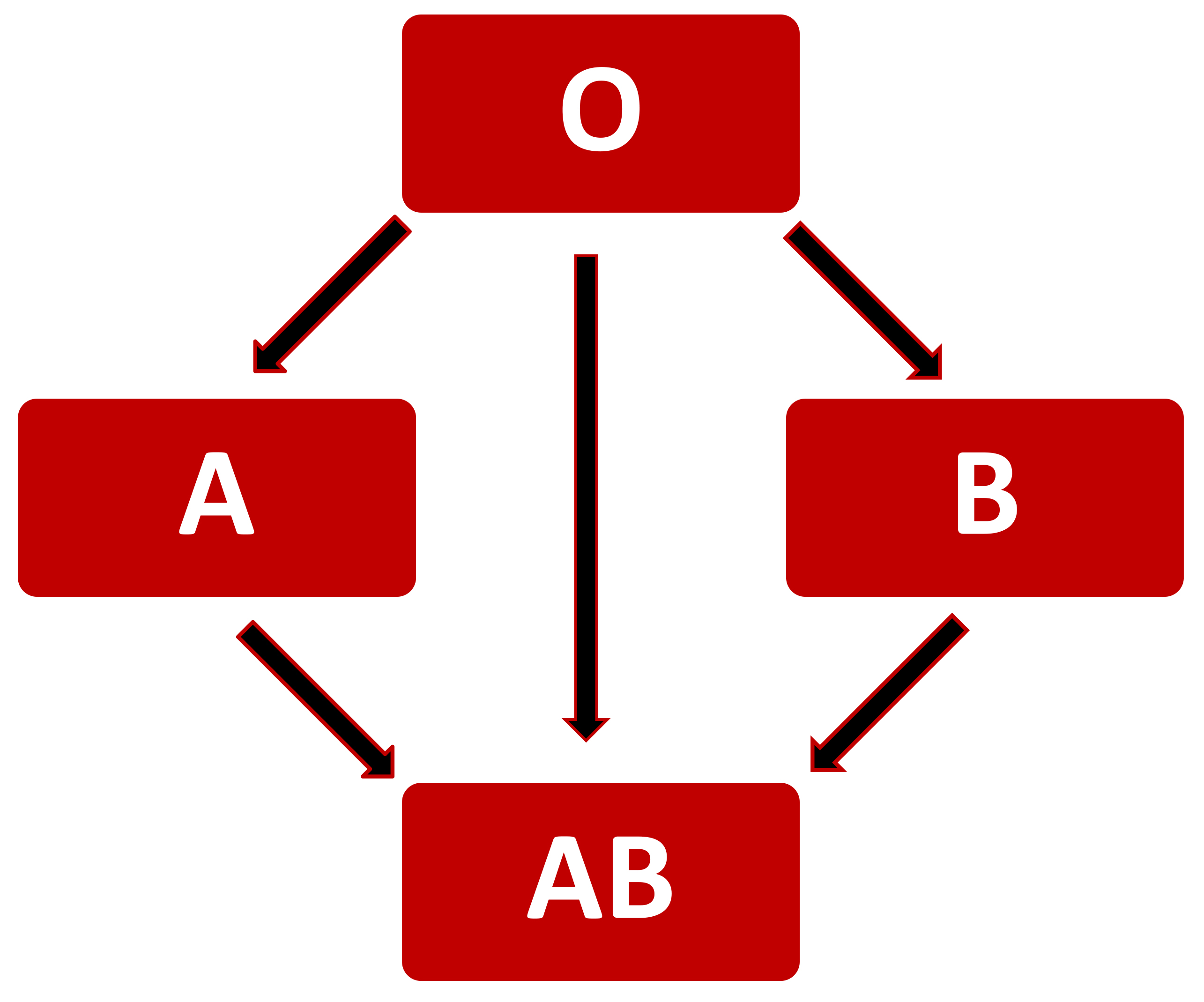
The four blood types are defined according to antigens present on the red blood cell surface.
- Type A blood has type A antigens
- Type B blood has B antigens
- Patients with type B blood have antibodies against the A antigen
- Type AB has both antigens
- No antibodies
- Type O has no antigens
- Patients with no antigens on their cells (type O blood) will have both Anti - A and Anti-B antibodies in the plasma
Patients with the Rhesus antigen (D) are Rh +, and those without it are Rh negative.
About 85% of the population is Rh +. Anti–Rhesus (D) antigens are absent in Rh+ patients.
This means that 70% of Rh-negative patients who get Rh+ blood will slowly develop anti-Rhesus antibodies after some time. So, the reaction between Rh+ and Rh-negative donor cells may take some time to develop and may not be apparent on first exposure. The subsequent exposure of a Rh-negative person to Rh+ blood may result in an acute hemolytic reaction.
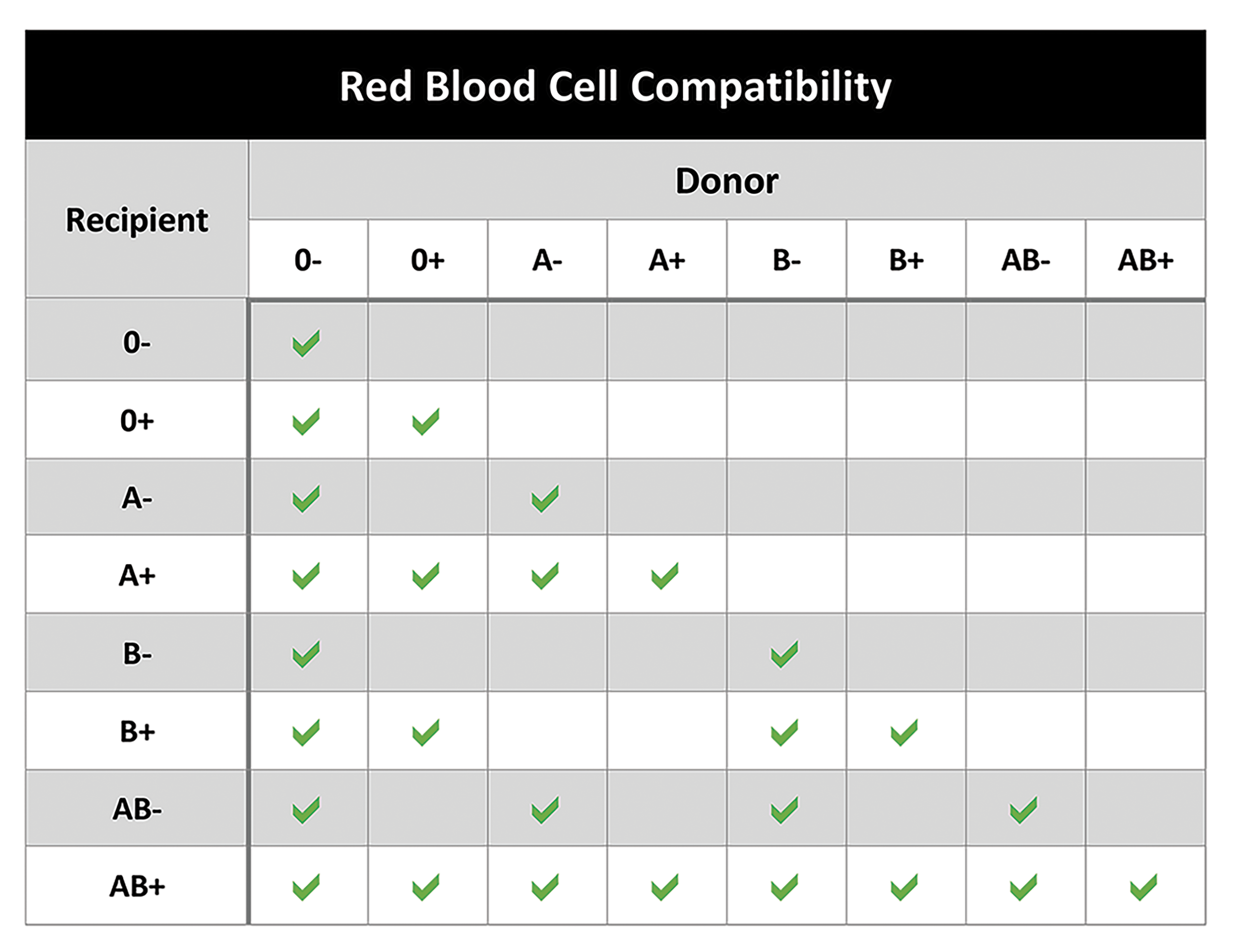
Blood component therapy
The recipient's reaction to antibodies with donor RBC antigens can activate the complement system and lead to intravascular hemolysis of the red cell.
Type O+ recipients (type O, Rh+) will have anti-A and anti-B antibodies but not anti-Rhesus antibodies.
These patients must not receive type A, B, or AB blood. They must receive type O blood, which may be Rh+ or negative.
Patients with type AB-negative (Type AB, Rh negative) will lack the A and B antibodies in their plasma and may not have the anti-Rhesus antibody.
- They can receive A-, B-, AB-, or O- blood
Individuals with the most antigens on their RBCs have the fewest antibodies and can receive all blood types (A+, A-, B+, B-, AB+, AB-, O+, O-).
- AB+ patients are universal recipients
Individuals with the fewest antigens on their cells (O-) have the most significant number of antibodies in their plasma, making them universal donors.
- Type O- patients are the universal donors