A small compilation of nurse anesthesia care plans
These anesthesia care plans are meant to inspire nurse anesthesia residents when they are making their care plans. Always make sure you fully understand and "own" your care plan. Your plan must be specific for your patient and should always be with the most up-to-date information.
Lumbar Fusion and Instrumentation, Posterior
Common Preoperative Diagnosis
Lumbar segmental instability
Spondylolisthesis - anterior displacement of the vertebra - may cause back pain, stiffness, and tightening of hamstrings
Iatrogenic lumbar instability - caused by outside influence
Lumbar disc disease
Spondylolysis - defect of vertebra
Mechanical back pain syndrome
Patients age 15 – 85 yrs., male: female 3:2
Various Approaches
Pedicle Screw Stabilization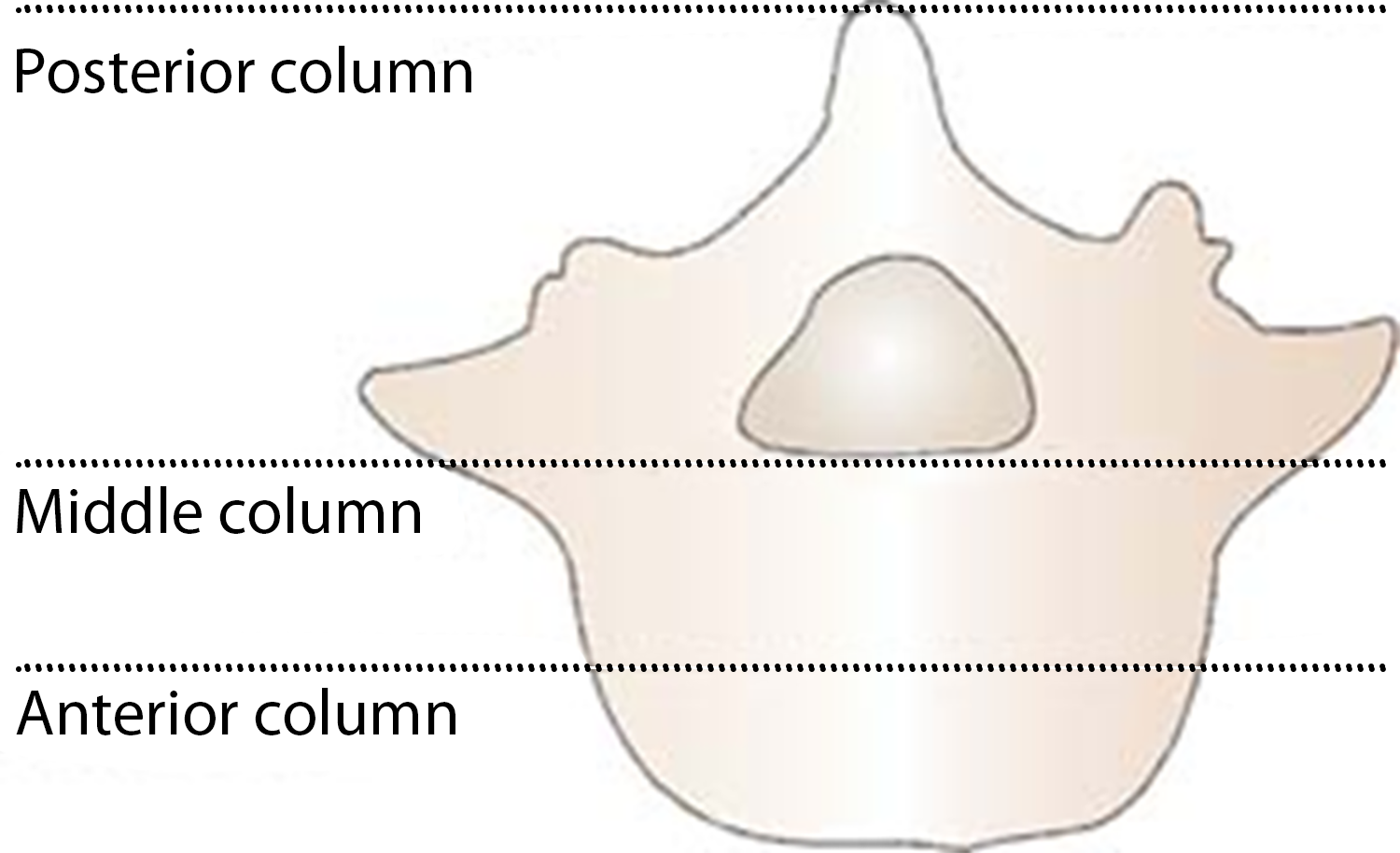
Provides rigid three-column spinal fixation - the preferred instrumentation mode in lumbar spinal surgery. Pedicle screws are passed after tapping the entry site, fixed with rods or plates on each side of each vertebral segment.
A major risk is screw malposition and nerve-root injury
Pedicle screws may be combined with hooks to provide fixation of the lumbar/thoracolumbar spine, which improves stability and minimizes the risk of instrumentation failure
Posterolateral Fusion (PLF)
Posterior midline incision with the paraspinal muscles retracted. Decompressive laminectomy and discectomy as needed. Posterolateral fusion is performed by decorticating (removing the outer layer), the facet joints and transverse processes. The bone graft is then placed over the decorticated bone. Instrumentation with pedicle screws and plate/rod is often done for stability and to facilitate fusion
Posterior Lumbar Interbody Fusion (PLIF)
Bilateral laminectomy and removal of the inferior facet and the medial portion of the superior facet. The facet joints provide stability to the spine, allow the spine to bend and rotate, and keep the back from slipping forward. There is a thin layer of cartilage between the two joint surfaces to provide smooth and efficient movements.
The dural sac is retracted, and total discectomy with removal of cartilaginous end plates is performed. The anterior disk space is packed with bone graft. Bone graft is inserted into the posterior half of the disc space on both sides to provide structural support close to the center of rotation. Monitor nerve roots closely. Instrumentation with pedicle screws and a rod/plate is often added to facilitate early fusion and ambulation while preventing the extrusion of the graft. This procedure enables the achievement of combined anterior and posterior spinal fusion while avoiding the significant morbidity often associated with anterior lumbar surgery. The disadvantage is the risk of nerve root injury and compromise of facet joint integrity.
Preoperative Considerations
Mortality
0-5%
Morbidity
- Nonunion - 20-30%
- Nerve-root injury
- CSF leak
- Infection
- Significant blood loss
Pain Score
6-10
Surgical Time
2 hrs for single level + 0.5 hr for each additional level
Antibiotics
Cefazolin weight-based
Position
Prone for the posterior approach
This patient category may be difficult to position due to their spine issues
Will have to individualize and improvise to provide the best possible support and avoid pressure point issues
It may require a longer time for positioning
Prone Position
Preop assessment of head, neck, shoulder, and arm mobility
Heart ok as long as avoiding occlusive pressure on the inferior vena cava and femoral veins
Increased SVR, and PVR leading to decreased SV/CO/CI
Abdominal pressure may impede venous return due to compression of the inferior vena cava and aorta and increase surgical bleeding during spine surgery due to engorgement of epidural veins
Increased zone 3 a > v > A
Decreased TLC, and reduced compliance leading to increased work of breathing
Increased PIP to achieve adequate ventilation as the abdomen pushes up. Monitor for barotrauma
CNS damage is high risk - keep the neck in neutral
If head below heart level = blood/cerebrospinal fluid accumulates (remember no valves, gravitational flow) = increased ICP, decreased CPP
Risk of post-op blindness - lubricate pad eyes with op-site, gauze, and shield. Check eyes every 15 minutes during the case to ensure no pressure
LR max of 40ml/kg for total surgery to possibly minimize postop blindness from ischemic optic neuropathy; if additional fluid is needed, give hetastarch 6% up to 20ml/kg, albumin 5%, or blood.
Pressure Points to be Padded
- Torso typically supported on a frame or with rolls from shoulder to iliac crest/crosswise at pelvis and shoulders
- Lower legs supported with pillows
- UE either tucked or on arm boards with arms flexed at shoulder and elbow (know preop issues with joint mobility)
- The face must be padded and secured
- Be careful with forehead, eyes, cheeks, and chin
- Pad pressure points at elbows, knees, ankles, and genitalia
- Ensure limited pressure on nipples
Preoperative Anesthetic Considerations
Neurologic
Patients may present with motor weakness, sensory deficits, or bowel/bladder dysfunction
Make sure you document any issues. The patient may have had a preop MRI
Hematologic
High risk of blood loss. Patients need to have T&C done, with a minimum of 2 units of RPBCs available. Consider using a cell saver. Pts may have been on anticoagulants, which increases the risk of bleeding
Laboratory
Baseline BMP and H&H
Preoperative
More pain than other patient categories; may have had previous back surgeries. They may not have gotten their regular pain medication due to surgery. They may have anxiety due to prior surgeries
Medicate with versed and possibly a small dose of fentanyl
Placement of A-line in preop holding or in OR after induction along with placement of CVP line
Possible use of Jackson table.
Anesthetic Considerations
ERAS protocol, limit NPO duration, alcohol, and smoking cessation. Review nutritional status and discuss post-operative pain management. Consider using goal-directed therapy for fluid management.
Blood conserving strategies
Autologous blood donation before surgery if medically stable
- Still, risk of infection, more costly, may go to waste, risk of perioperative anemia, and an increased risk of transfusion
Cell saver if there is no risk of contamination
- Urine, cancer, bone fragments, bowel contents, infection, malignancy, sickle cell disease, clotting agents
Acute normovolemic hemodilution
If blood transfusion - 1 unit PRBC increases Hb 1g and Hct 2-3%
If mass transfusion, consider the need for FFP, platelets, cryoprecipitate (clotting factors)
- Risk of hypothermia, hypervolemia, elevated K+ levels, decreased 2,3 DPG levels (so need increased O2 delivery), dilutional coagulopathy (due to limited plasma in RPBC), acid-base changes with prolonged storage (reduced pH), and citrate intoxication (CPDA preservative - citrate/phosphate/dextrose/adenine)
Complications
Hypotension - due to vascular injury
Nerve root injury
Lung tissue injury - may need a chest tube
Blindness
Renal compromise
Bowel compromise