A small compilation of nurse anesthesia care plans
These anesthesia care plans are meant to inspire nurse anesthesia residents when they are making their care plans. Always make sure you fully understand and "own" your care plan. Your plan must be specific for your patient and should always be with the most up-to-date information.
Nipple Reconstruction
Etiology
Breast cancer is the second most common cancer in women after skin cancer. Of breast cancer patients in 2008, according to the American Society of Plastic Surgery, approximately 80.000 women underwent breast reconstruction
Types of reconstruction
Immediate reconstruction may be contraindicated if radiation treatment is planned
Prosthetic reconstruction with a temporary tissue expander or a saline-filled implant placed behind the pectoral muscle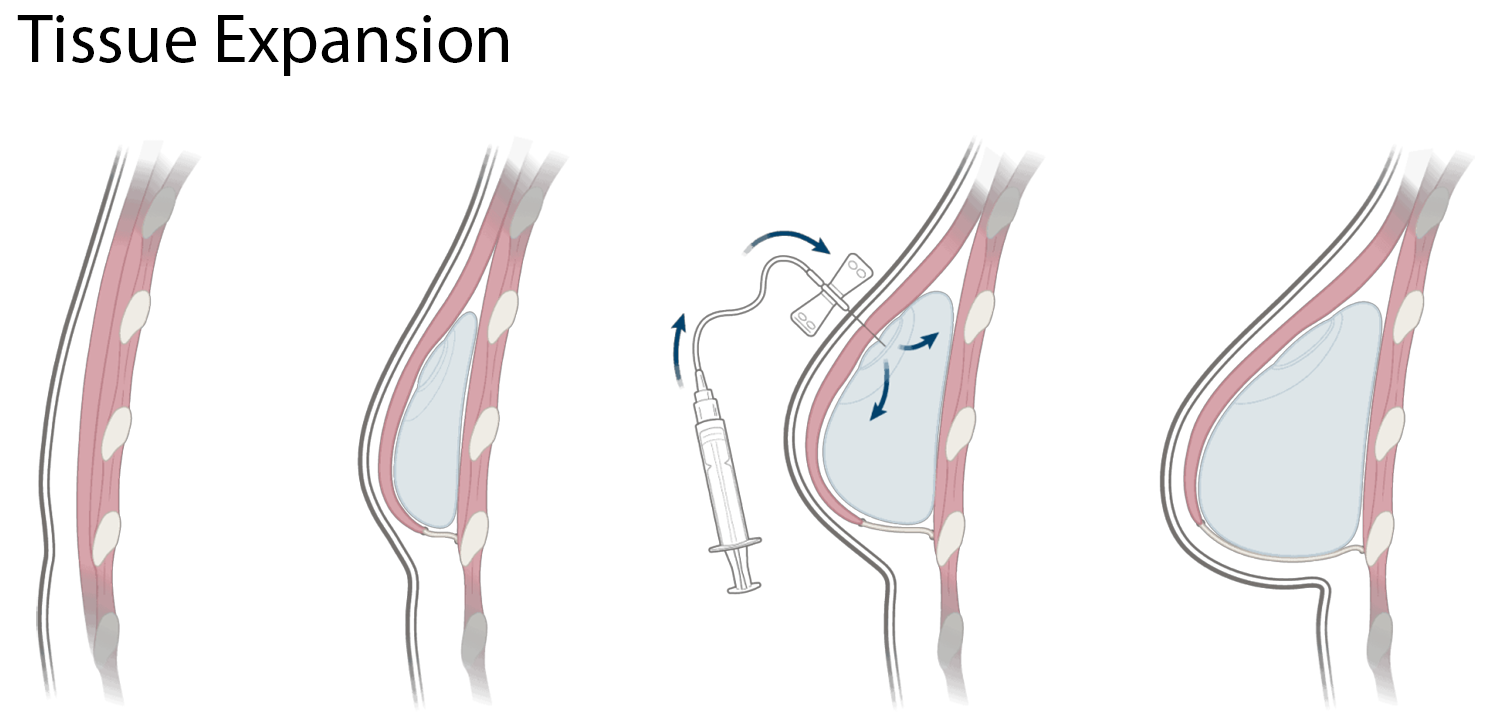
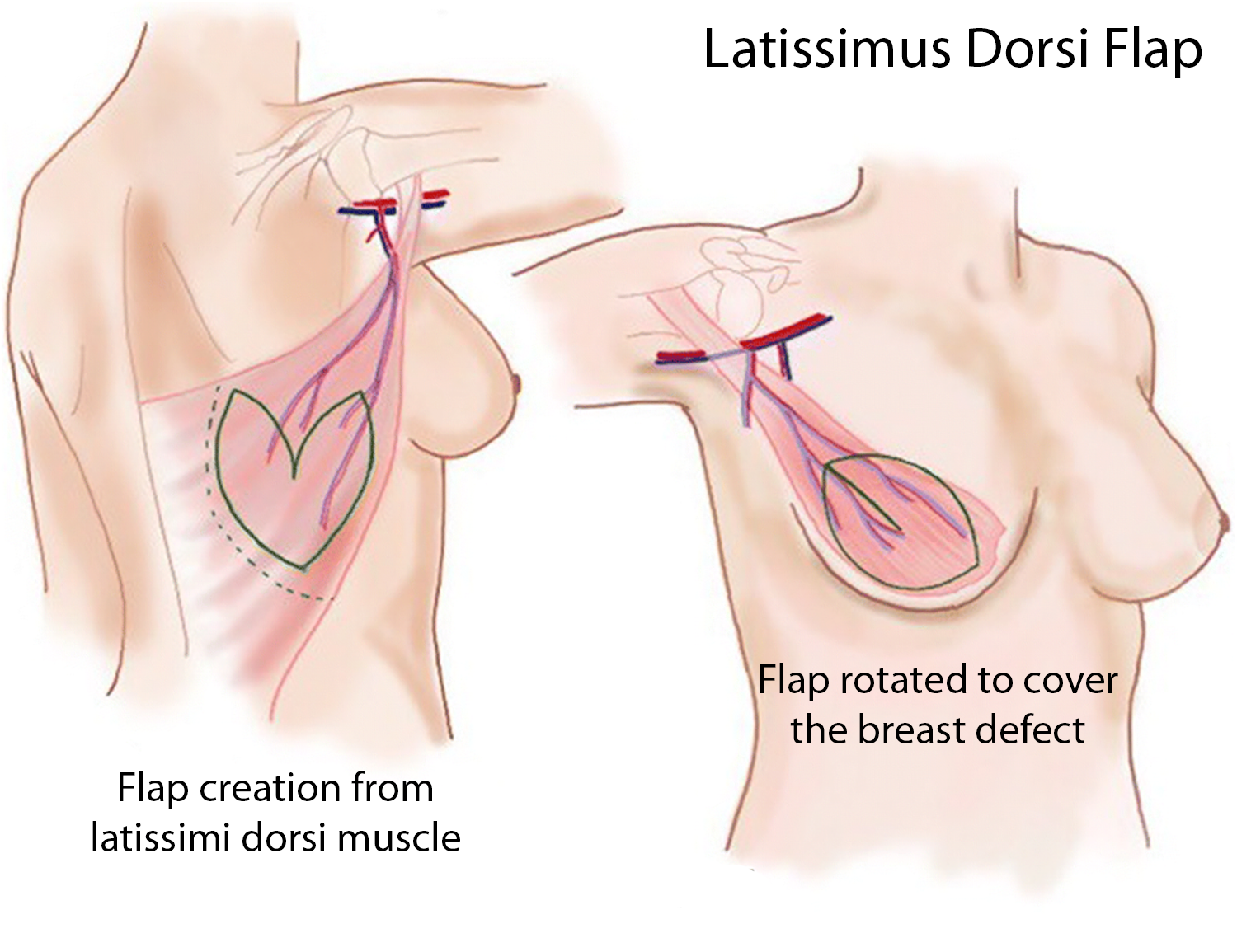 Autologous breast reconstruction - latissimus dorsi myocutaneous flap is muscle from the back with skin rotated to the anterior chest for the creation of breasts and often involves the use of a breast implant to create volume
Autologous breast reconstruction - latissimus dorsi myocutaneous flap is muscle from the back with skin rotated to the anterior chest for the creation of breasts and often involves the use of a breast implant to create volume
Another option is a Transverse Rectus Abdominis Myocutaneous - TRAM flap - an ellipse of abdominal skin and subcutaneous tissue based on the rectus abdominus muscle. Blood supply is maintained with superior epigastric and inferior epigastric arteries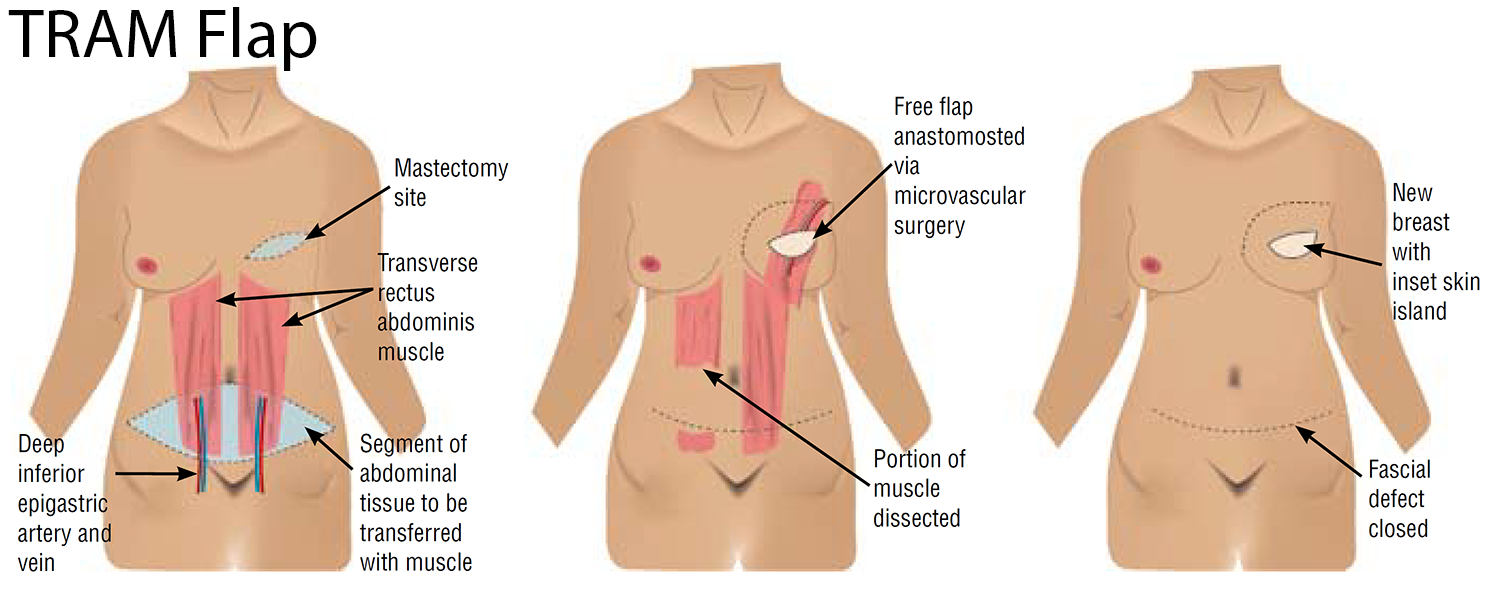
Nipple reconstruction is usually the last part to be completed and is considered necessary for the patient's psychological well-being. Traditionally performed once the reconstructed breast has settled in. Various techniques, from skin tattooing to reconstruction of the nipple using tissue from other areas of the body
Reconstruction of position, size, shape, and color of the native nipple-areola complex currently are attainable goals; functional restoration of erectile ability and erogenous sensation are goals for future reconstructive surgeons. It is vital to use the opposite nipple as a guide if present; if not, it is essential to mark when the is awake in a sitting position for optimal results
Complications related to poor blood supply can be prevented by creating a nipple that is 20-30% larger than the contralateral nipple if applicable
Preoperative Considerations
Patient Population
Mostly female 30-70 years
Associated Conditions
Breast cancer, cardiovascular disease, post-chemotherapy (know what drugs and last treatment), pulmonary disease
Position
Supine
- May need to temporarily change to sitting for evaluations during the reconstruction
Keep the head in a neutral position
Massage/reposition the head during lengthy procedures to prevent alopecia
Heels off mattress for more prolonged procedures
Padding
Protect pressure points. Arms either with hands supinated <90degree (prevent Brachial Plexus injury from stretch) or alongside with hands facing body. Pad to prevent ulnar nerve injury. Possible pillow under knees if hx of back pain, maintain the lordotic curve in the spine, and avoid tension on the sciatic nerve. Prevent alopecia with padding of the head.
Check eyes - always tape them to prevent corneal abrasion
Monitors
Pulse ox, ECG, NIBP, temp, Bair hugger (lower), PNS if muscle relaxant
Incision
Depending on the technique employed
Surgical Time
1-2 hrs
Preoperative Area
Verify NPO, consent signed, questions answered
If any chemotherapy history, try to find out about drugs
- Bleomycin - pneumonitis, pulmonary fibrosis
- Cisplatin - renal failure
- Cyclophosphamide - plasma cholinesterase inhibition, hemorrhagic cystitis, acute delirium
- Doxorubicin - cardiomyopathy
- Methotrexate - renal failure, irreversible dementia
- Vincristine - peripheral and autonomic neuropathy
Antibiotics
Per surgeon
Physiologic Changes
Decreased FRC and HR
Increased venous return, leading to increased preload and CO
Increased intraabdominal pressure
Zone 3 (a-v-A) in the dorsal portion of the lungs
CNS
Blood/cerebrospinal fluid drainage is gravity dependent, valve less; when supine = increased ICP, which decreases cerebral perfusion pressure (CPP= MAP-ICP/or CVP).
If BMI is elevated - decreased FRC. Difficulty maintaining tidal volumes due to body weight pressing down on the chest
Postoperative Complications
Partial and total loss of nipple
Epidermolysis (development of blisters in the skin)
Loss of nipple projection
Discoloration
Anesthesia
General with ETT if muscle relaxation is needed
Induction
Preoxygenation
Lidocaine 1 mg/kg/IV
Propofol 1-2 mg/kg/IV - consider etomidate 0.1-0.4 mg/kg/IV if cardiac disease - note myoclonus and adrenocortical suppression
Fentanyl 1-3 mcg/kg/IV
Succinylcholine 0.5-1.5 mg/kg/IV
Maintenance
Isoflurane - if smoker use sevoflurane
Fentanyl
If a muscle relaxant is needed, consider atracurium 0.3-0.5 mg/kg/IV
- Not for asthma pts (histamine release)
Emergence
Zofran IV
Neostigmine and glycopyrrolate for reversal if use of muscle relaxant
Anesthetic Considerations
Maintain blood pressure to avoid a decrease in blood supply to the nipple
Possible chemotherapy drug implications