A small compilation of nurse anesthesia care plans
These anesthesia care plans are meant to inspire nurse anesthesia residents when they are making their care plans. Always make sure you fully understand and "own" your care plan. Your plan must be specific for your patient and should always be with the most up-to-date information.
Ophthalmic anatomy
The eye has six extraocular muscles
Cranial nerves and eye anatomy
CN 2 - Optic nerve
Receives information from the retina, carries retinal artery and vein into the globe
CN 3 - Oculomotor nerve
Innervates superior and inferior rectus muscles, the inferior oblique muscle, the medial rectus muscle, and the levator muscle of the upper eyelid
Parasympathetic fibers to the ciliary ganglion, which causes constriction of iris sphincter muscles
Sympathetic fibers from the carotid artery plexus cause contraction of the radial muscles and lead to papillary dilation
CN 4 - Trochlear nerve
Motor fiber to the superior oblique muscle (rotates eye toward the nose)
CN 5 – Trigeminal nerve
Sensory and motor
- Ophthalmic (pain, touch, temp to eye structures)
- Maxillary (pain, touch, temp to upper lip, nasal mucosa, and scalp muscles)
- Mandibular nerves
CN 6 – Abducens nerve
Motor function to the lateral rectus muscle
CN 7 - Facial nerve
Motor to face - To Zanzibar By Motor Car" (part of CN VII)
- Temporal (frontal) branch of the facial nerve
- Zygomatic branch of the facial nerve
- Buccal branch of the facial nerve
- Marginal mandibular branch of the facial nerve
- Cervical branch of the facial nerve
The Temporal and Zygomatic branches are most important for eye surgery
CN X – Vagus nerve
Efferent pathway for the oculocardiac reflex, which can result in bradycardia and dysrhythmias
Oculocardiac reflex
Trigeminal-vagal reflex generated by pressure to the globe, the optic nerve or the conjunctive, or by traction on the extraocular muscles.
The afferent pathway runs through the ciliary nerves to the ciliary ganglion, then along the ophthalmic division of the trigeminal nerve to the base of the 4th ventricle.
The efferent pathway is via the Vagus nerve to the cardio-inhibitory center.
This is most often seen in children getting eye muscle procedures.
Acute sinus bradycardia but may also see other arrhythmias.
Treatment
Surgeon to release pressure immediately
Assess oxygenation and ventilation
May need Atropine 2-3mg
Can pretreat with Glycopyrrolate or atropine just before surgery
The symptoms can reappear but seems to be fatigued with continued manipulations
Complications from eye surgery
Corneal abrasions due to drying of the exposed cornea or from direct trauma
Movement during ocular surgery is the most common mechanism of injury
Coughing and bucking.
Consider muscle relaxants
Chemical injury from cleaning materials Eddy
Lens
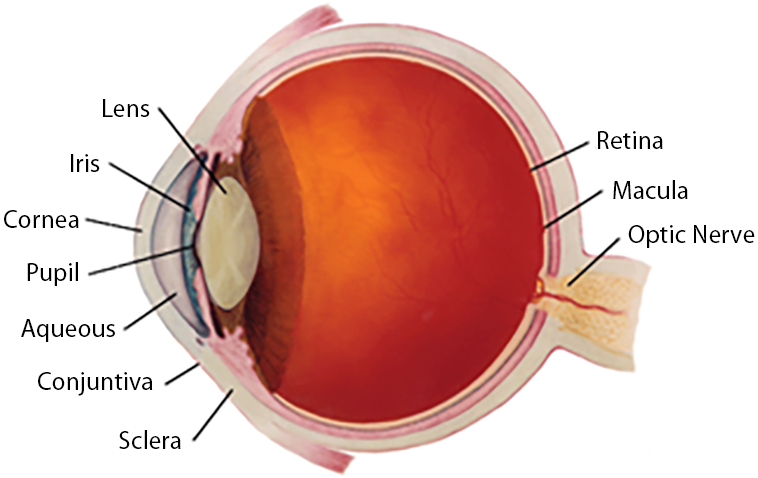 Located just behind the iris, the lens is one of the components that determines how the eye is focused and is also responsible for allowing the eye to see near objects. As we age, the lens becomes increasingly dense and inflexible, causing a continual decrease in the eye's focusing ability, known as presbyopia. The lens can develop cataracts due to age or injury or be present at birth.
Located just behind the iris, the lens is one of the components that determines how the eye is focused and is also responsible for allowing the eye to see near objects. As we age, the lens becomes increasingly dense and inflexible, causing a continual decrease in the eye's focusing ability, known as presbyopia. The lens can develop cataracts due to age or injury or be present at birth.
Iris
This is the ring-shaped colored part of your eye and is responsible for controlling the amount of light that enters the eye. In the light, the iris constricts to make the opening in the iris, the pupil, smaller to decrease the amount of light entering the eye. In the dark, the iris dilates, increasing the pupil size and allowing more light to enter the eye.
Cornea
The cornea is a clear dome over the iris and is, on average, just 1/2 mm thick. It is one of the components that determines how the eye is focused. Contact lenses are worn on the cornea, and laser refractive surgery is performed here.
Pupil
This is the circular opening in the center of the iris, and it changes size in different lighting conditions. The pupil is usually black, but if the eye is lit up inside, such as when a camera flashes, the color of the eye's interior will be visible, and the pupil will appear red.
Aqueous
This fluid fills the area between the cornea and the lens and is continually produced and drained. The amount of aqueous in the eye determines the eye pressure, which varies at different times and on different days. If the eye pressure is too high for the eye tissues to tolerate, glaucoma can develop.
Conjunctiva
This thin layer of transparent tissue covers the white of the eye, the sclera. The conjunctiva contains many blood vessels, which fill with blood and expand if the eye is irritated, making the eye appear red.
Sclera
This is the white, tough outer casing of the eye, which gives the eye its shape and strength to resist damage.
Vitreous
This jelly-like fluid fills the area between the lens and the retina. Often, the vitreous contains fibers or clumps, which are seen as shifting black or translucent shapes in the vision and are called floaters. It is expected to notice an increase in floaters over time. The vitreous is contained within a capsule, attached to the retina at multiple points. At some point in life, usually in the 50s or 60s, the capsule of the vitreous pulls away from the retina and collapses into itself, much like a balloon deflating. This is called a vitreous detachment and is a normal part of aging.
Retina
This thin layer of tissue lines the inside of the eyeball and contains cells that receive light and transfer it into visual messages sent to the brain via the optic nerve. The retina also contains many blood vessels, which can break and bleed due to various eye conditions or diseases, causing vision loss. A retinal detachment occurs if the retina loses its attachment to a part of the eyeball, allowing it to come away from the wall of the eye.
Macula
This is an area in the central part of the retina that provides detailed vision. Diseases or injuries affecting this area almost always cause noticeable vision loss. Macular degeneration is one of the most common diseases affecting this part of the retina.
Optic Nerve
This nerve carries visual messages from the retina to the brain, interpreting them and perceiving vision. Glaucoma damages the optic nerve, causing individual nerve fibers to gradually die off, resulting in a subtle but progressive loss of vision.