A small compilation of nurse anesthesia care plans
These anesthesia care plans are meant to inspire nurse anesthesia residents when they are making their care plans. Always make sure you fully understand and "own" your care plan. Your plan must be specific for your patient and should always be with the most up-to-date information.
Sickle Cell Disease
Etiology
Inherited hemoglobinopathies range in severity from benign sickle cell trait to debilitating sickle cell anemia
 Abnormality in globin genes in hemoglobin
Abnormality in globin genes in hemoglobin
- If both genes are the same, the organism is homozygous for the trait
- Homozygous disorder seen in 0.5-1% of African Americans
- If both genes are different, the organism is heterozygous for that trait
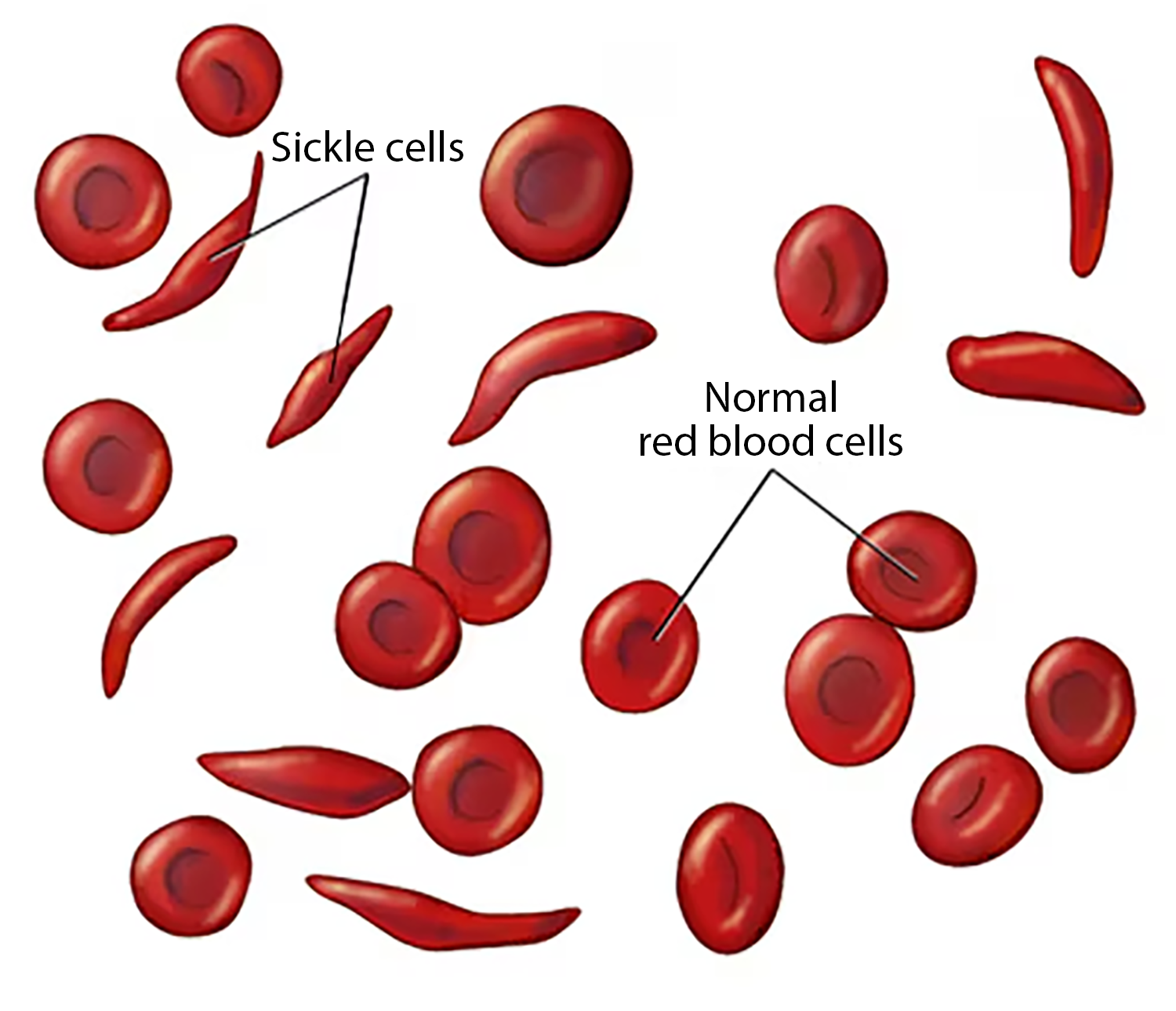
Normal RBCs live for 120 days and contain hemoglobin A
Sickle cells contain hemoglobin S (sickle) or hemoglobin C, both abnormal and only live about 16 days
Sickle cells are stiff, distorted shapes and have difficulty passing through smaller vessels
RBCs of African Americans who are homozygous for Hgb S contain 70-98% Hgb S
- The development of sickle cell anemia is a risk
- Chronic hemolysis and acute episodic vasoocclusive crises that may cause organ system failure
Sickling seen with PO2 of 30 to 40
The sickle cells also block the flow of blood through vessels, resulting in lung tissue damage (acute chest syndrome), pain episodes (arms, legs, chest, and abdomen), stroke, and priapism (painful, prolonged erection). It also causes damage to most organs, including the spleen, kidneys, and liver. Damage to the spleen makes sickle cell disease patients, especially young children, easily overwhelmed by certain bacterial infections
Sickle Cell Crisis
A sickle cell crisis may be caused by
- Decrease in oxygen saturation
- Decrease in temperature
- Infections
- Dehydration
- Stasis
- Acidosis
Perioperative mortality of 10% and postoperative mortality of 50%
The preop goal of Hct 30% helps prevent postop complications, but minor procedures show little benefit from transfusion
Note
These patients will take a 1 mg dose of folic acid daily for life (essential for red blood cell production)
From birth to five years of age, they will also have to take penicillin daily due to the immature immune system that makes them more prone to early childhood illnesses
Pneumococcal sepsis is the leading cause of death among infants b/c a damaged spleen cannot clear pneumococci from blood - administer antibiotics
Sickle Cell Trait
A condition in which there is one gene for the formation of sickle hemoglobin and one for the formation of normal hemoglobin
Usually, people with sickle cell traits do not have any medical problems, and they can lead a normal life
- They do not develop sickle cell disease
It’s important to know if you have the trait because if both parents have sickle cell trait, then there is a 25% chance with each pregnancy that the child will have sickle cell disease
Pediatrics
The sickling of the RBCs is prominent, and symptoms begin around six months as the fetal hemoglobin decreases
Anesthetic considerations
Standard ASA monitors
Consider regional versus general anesthesia
Hydration is usually 1.5x maintenance if the renal status is OK
Maintain normocapnia
At least 50% inspired O2 concentration
- Maintain O2 sat >95% at all times
Transfuse, if necessary, avoid getting Hb >1 g/dl
- Think of viscosity as it increases the risk of end-organ damage
Maintain normothermia
- Warm room
Aggressive pain management postop is critical due to surgical as well as sickle pain
- Pain can worsen complications of the disease
Complications
Age, frequency of hospitalizations/transfusions for episodes of crisis, evidence of organ damage such as low baseline O2 sat, elevated Cr, cardiac dysfunction, hx of CNS events, or concurrent infection
A frequently used mnemonic for sickle cell crisis is HBSS PAIN CRISIS
- H - Hemolysis, hand-foot syndrome
- B - Bone marrow hyperplasia/infarction
- S -Stroke: thrombotic or hemorrhagic, subarachnoid bleeds
- S - Sequestration crisis involving spleen or liver
- P - Pain episodes, priapism (prolonged erection), psychosocial problems
- A - Anemia, aplastic crisis, avascular necrosis
- I - Infections: CNS, pulmonary, GU, bone, Joints
- N - Nocturia, urinary frequency from hyposthenuria (low specific gravity)
- C - Cholelithiasis, cardiomegaly, congestive heart failure, chest syndrome
- R - Retinopathy, renal failure, renal concentrating defects
- I - Infarction: bone, spleen, CNS, muscle, bowel, renal
- S - Skin ulcers (primarily leg)
- I - Increased fetal loss during pregnancy
- S - Sepsis