A small compilation of nurse anesthesia care plans
These anesthesia care plans are meant to inspire nurse anesthesia residents when they are making their care plans. Always make sure you fully understand and "own" your care plan. Your plan must be specific for your patient and should always be with the most up-to-date information.
Spinal Fusion Anterior - Posterior
Usual Preop Diagnosis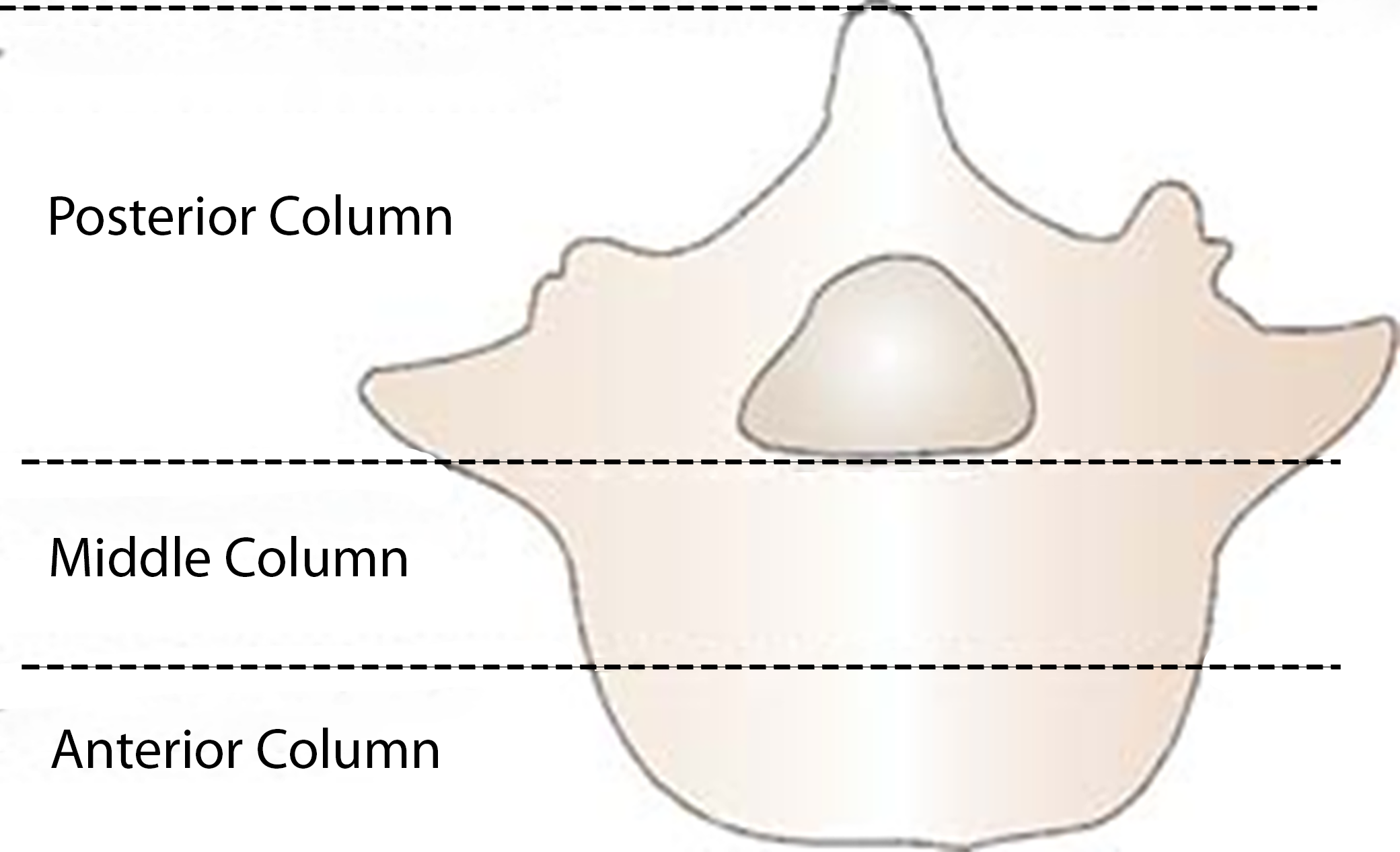
Lumbar segmental instability
Spondylolisthesis - anterior displacement of the vertebra - may cause back pain, stiffness, tightening of hamstrings
Iatrogenic lumbar instability - caused by outside influence
Spondylolysis - defect in vertebra
Mechanical back pain syndrome
Pts' age from 15-85 yr old, male: female 3:2
Patients may present with multilevel vertebral collapse, unstable three-column injuries, severe kyphosis (forward bend, think lung expansion), scoliosis (abnormal curving of the spine), and/or neoplastic or infective conditions involving multiple spinal levels requiring combined anterior and posterior instrumentation, which provides 
- Complete circumferential neural decompression
- Provides maximal neuronal recovery
- Rigid short-segment spinal fixation
- Facilitates early ambulation with minimal orthotic support
- Maximal correction of deformities
- Low instrumentation failure and high fusion rates
- Combined approach
- Greater possibility for complete resection of neoplastic or infective tissue
- Combined anterior-posterior instrumentation can be used to leverage each other for deformity correction
- The picture shows the thoracic pedicle screws and rods used for stabilization
- If a posterior thoracic approach is used, the field will be filled with saline to check for any leaks at the end of the procedure
Use of fluoroscopy - wear protective lead during the procedure
Preoperative Considerations
EBL
500-5000 mL
Mortality
0-3%
Morbidity
Respiratory problems such as atelectasis and pneumonia
Infection
Wound breakdown
Bone graft dislodgement
Significant blood loss
Pain Score
7-10
Surgical Time
4-10 hr
Antibiotics
Cefazolin weight-based
Position
Anterior Part - Supine
Supine for anterior approach, prone for posterior approach
This patient category may be difficult to position due to their spine issues. Individualize and improvise to provide the best possible support and avoid pressure point issues. Positioning may take longer.
Keep the head in a neutral position
Massage/reposition the head during lengthy procedures to prevent alopecia
Heels off mattress for more prolonged procedures
Decreased FRC and HR
Increased venous return, leading to increased preload and CO
Increased intraabdominal pressure
Zone 3 (a>v>A) in the dorsal portion of the lungs
CNS: blood/cerebrospinal fluid drainage is gravity dependent, valve less; when supine = increased ICP, which decreases cerebral perfusion pressure (CPP = MAP-ICP/or CVP)
If BMI is elevated - decreased FRC. Difficulty maintaining tidal volumes due to body weight pressing down on the chest.
Padding: Protect pressure points. Arms either with hands supinated <90 degrees (prevent Brachial Plexus injury from stretch) or alongside with hands facing body. Pad to prevent ulnae nerve injury. Possible pillow under knees if hx of back pain, maintain the lordotic curve in the spine, and avoid tension on the sciatic nerve. Prevent alopecia with padding of the head.
Check eyes - always tape them to prevent corneal abrasion
Careful transition between anterior and posterior procedure to minimize disruption of the instrumentation
Posterior Part - Prone
Preop assessment of head, neck, shoulder, and arm mobility
Heart ok as long as avoiding occlusive pressure on the inferior vena cava and femoral veins
Increased SVR and PVR leading to decreased SV/CO/CI
Abdominal pressure may impede venous return due to compression of the inferior vena cava and aorta and increase surgical bleeding during spine surgery due to engorgement of epidural veins
Increased Zone 3, a>v>A
Decreased TLC and decreased compliance leading to increased work of breathing
Increased PIP to achieve adequate ventilation (abdomen pushes up). Monitor for barotrauma
CNS damage is high risk - keep the neck in neutral
If head below heart level = blood/cerebrospinal fluid accumulates (remember no valves, gravitational flow) = increased ICP, decreased CPP
Risk of post-op blindness – lubricate, pad eyes with op-site, gauze, and shield. Check eyes every 15 min during the case to ensure no pressure.
LR max of 40 mL/kg for total surgery to possibly minimize postop blindness from ischemic optic neuropathy; if additional fluid is needed, give hetastarch 6% up to 20 mL/kg, albumin 5%, or blood (Jaffy)
Pressure points to be padded
The torso is typically supported on a frame or with rolls from shoulder to iliac crest / crosswise at the pelvis and shoulders
Lower legs supported with pillows
UE either tucked or on arm boards with arms flexed at shoulder and elbow (know preop issues with joint mobility)
Pad pressure points at elbows, knees, ankles, and genitalia. Ensure limited pressure on nipples.
Anesthetic Considerations
Preop
Neurologic
Patients may present with motor weakness, sensory deficits, or bowel/bladder dysfunction. Make sure you document any issues. The patient may have had a preop MRI.
Hematologic
There is a high risk of blood loss. The patients must have T&C done, and at least two units of RPBCs should be available. Consider using a cell saver. The patients may have been on anticoagulants, increasing the bleeding risk.
Laboratory
Baseline BMP and H&H
More pain than other patient categories; may have had previous back surgeries. They may not have gotten their regular pain medication due to surgery. They may have anxiety due to prior surgeries
Medicate with versed and possibly a small dose of sufentanil
Placement of A-line in preop holding or in OR after induction along with placement of CVP line
Possible use of Jackson table.
Monitors
Pulse ox, ECG, NIBP, temp, Bair hugger, PNS, A-line, ?CVP, 2 large bore IVs, Foley Cath
Intraoperative
Induction
Preoxygenation
Pretreat with Rocuronium 3-5 mg IV
Lidocaine 1 mg/kg/IV
Propofol 1-2 mg/kg/iv - if cardiac disease, consider Etomidate 0.1-0.4 mg/kg/IV
Sufentanil 5-10 mcg IV
Succinylcholine 0.5-1.5 mg/kg/IV
ETT
If the thoracic approach may need DLT (double lumen tube) to facilitate one-lung ventilation
Maintenance
If using evoked potentials, consider TIVA - Propofol 75-200 mcg/kg/min and remifentanil (0.1-0.5 mcg/kg/min) - May see bradycardia (especially with Vecuronium), chest rigidity, respiratory depression, and decreased sympathetic tone: onset 30 sec, peak 3-5 min, duration of action 5-10 min (esterase elimination). Make sure to start post-op pain management toward the end of the case
If no evoked potentials - isoflurane, vecuronium (0.025mg/kg) or Pancuronium (0.02 mg/kg), sufentanil
Monitor K, Hct if excessive bleeding. ABGs as needed.
Emergence
Supine position
Evaluate facial and airway edema - consider length of surgery - may need overnight intubation
Zofran 4 mg IV
Decadron 4-6 mg IV
Document neurological status, if possible, before/when reaching the PACU
Complications
Hypotension - due to vascular injury
Nerve root injury
Lung tissue injury - may need a chest tube
Blindness
Renal compromise
Bowel compromise
Volume Considerations
Fluid replacement
EBV- male 75 mL/kg, female 65 mL/kg
- Weight in kg x male/female mL = EBV
Use ERAS protocol is applicable
EBL - replace with crystalloid 3:1 or blood 1:1
Allowable blood loss depends on medical history, including cardiac issues - (to Hb 10 or Hct of 30-35%)
Calculation EBV x (initial Hct-end Hct)/initial Hct gives you allowable blood loss
Blood Conserving Strategies
Autologous blood donation before surgery if medically stable
Cell saver if there is no risk of contamination
- Urine, cancer, bone fragments, bowel contents, infection, malignancy, sickle cell disease, clotting agents
Acute normovolemic hemodilution
If blood transfusion - I unit RPBC increases Hb 1 g and Hct 2-3%
If mass transfusion, think of the need for FFP, platelets, cryoprecipitate (clotting factors) - risk of hypothermia, hypervolemia, elevated K levels, decreased 2,3 DPG levels (so need increased O2 delivery), dilutional coagulopathy (due to limited plasma in RPBC), acid-base changes with prolonged storage (decreased pH), and citrate intoxication (CPDA preservative - citrate - phosphate - dextrose - adenine)
Hypotensive Technique
Deliberate hypotension
- Decrease blood flow, decrease blood loss, better visual in the surgical field, decrease blood transfusions - need A-line to monitor closely
Techniques
- Hypovolemia
- Volatile agents (decreased SVR/BP)
- Vasodilators (NGT/Nipride)
- Calcium channel blockers
- Cardene 5 mcg/kg/min / Cleviprex 1-2 mg/hr - NOTE: looks like Propofol
Use Isoflurane - minimal effect on CO decreases SVR, cerebral protection at low levels
Maintain MAP within 20-30% of preop
- Considering medical history - the brain needs MAP >50, GFR maintained with MAP >75, but renal parenchyma perfused at MAP in the 60s
This may inhibit Hypoxic Pulmonary Vasoconstriction (internal protection in hypoxia, where the lungs redirect blood flow to well-oxygenated areas), leading to increased dead space, intrapulmonary shunt, and PaCO2.
Anesthesia > 1 MAC and vasodilators inhibit HPV (Cardene has the least effect on HPV)
Risk of necrotic bowel with hypotension and hemodilution
Risk of post-op vision loss - visual deficits, rarely blindness
Patient medical history dictates how much hypotension they can tolerate
Once bony dissection is complete, there is less advantage to the hypotensive technique