A small compilation of nurse anesthesia care plans
These anesthesia care plans are meant to inspire nurse anesthesia residents when they are making their care plans. Always make sure you fully understand and "own" your care plan. Your plan must be specific for your patient and should always be with the most up-to-date information.
Thyroidectomy
Etiology
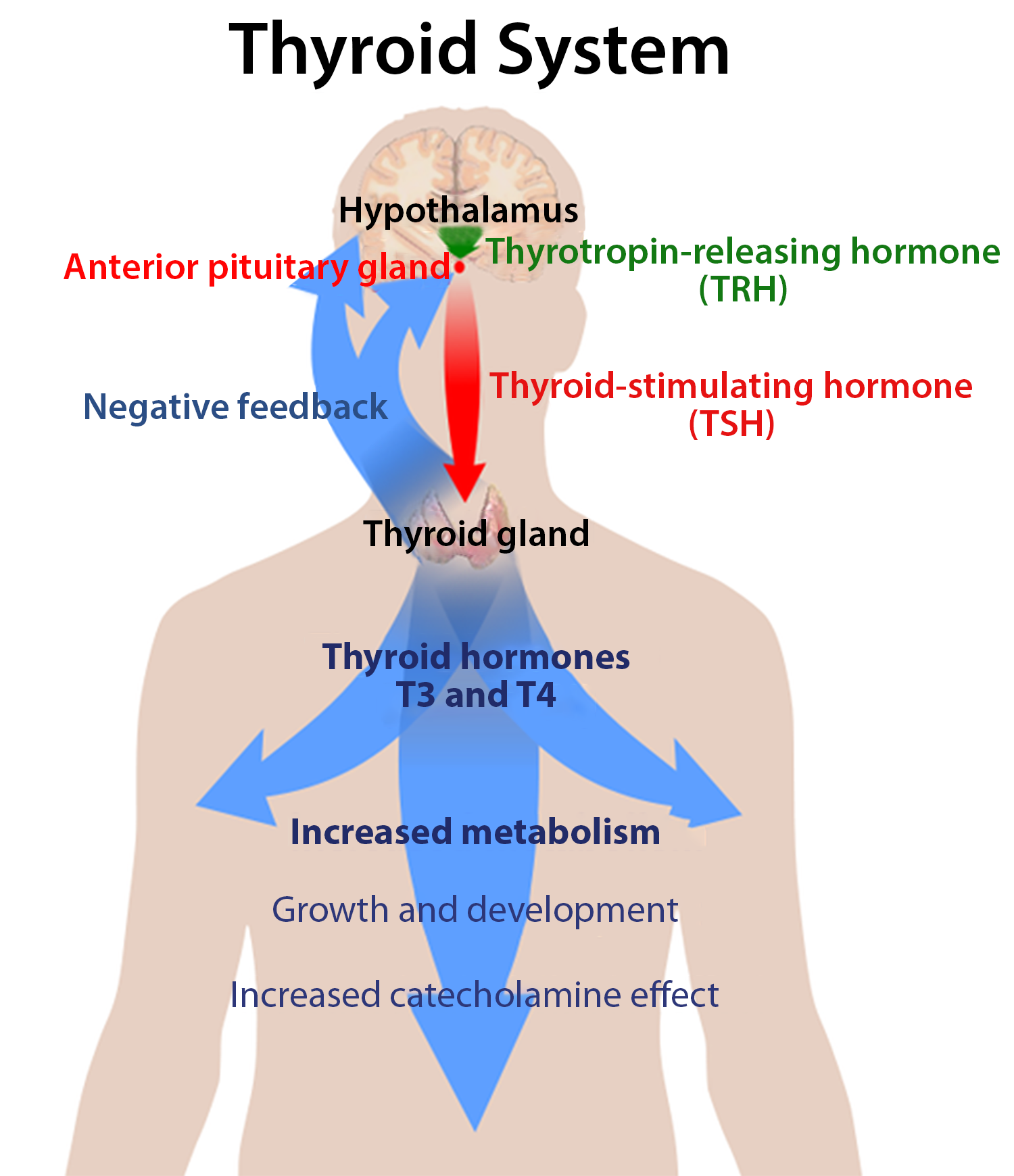
Thyroid hormones are T4 and T3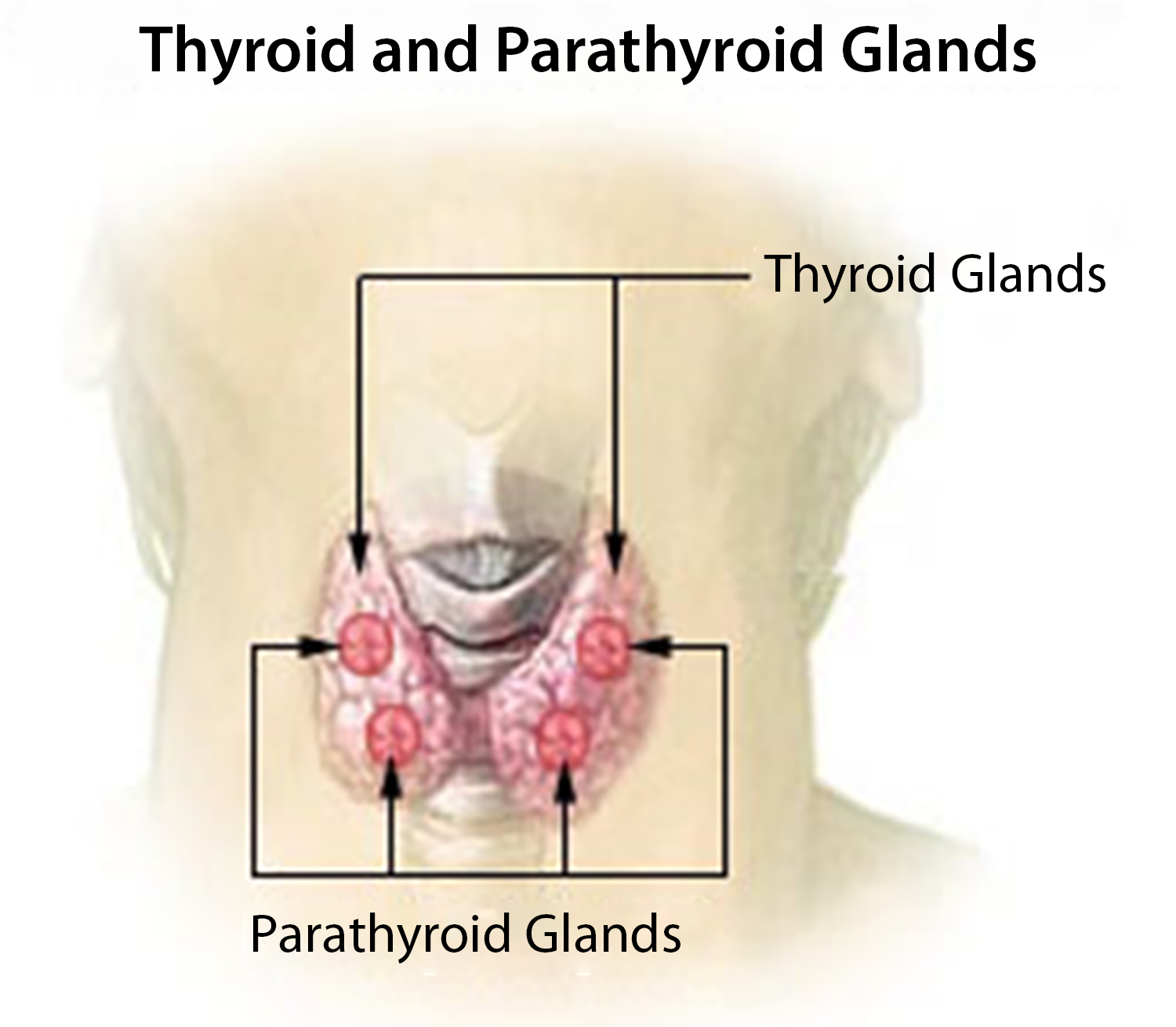
- T4 - Thyroxine - half-life of 6 days
- T3 - Triiodothyronine - half-life of one day
- rT3 is an inactive form of T3
T4 is the most prevalent, but T3 is the most potent and active form—ratio 4:1
Deiodinase enzyme converts T4 to T3 (from the liver/kidney and other tissues)
Thyroid hormones are synthesized in the follicular epithelial cells, and the follicular lumen stores newly synthesized thyroid hormones attached to thyroglobulin
TRH is released from the hypothalamus, stimulates the release of TSH from the anterior pituitary, and stimulates the thyroid gland to release T4 and T3—negative feedback to the anterior pituitary
Patients presenting for thyroid surgery are usually made euthyroid before elective surgery and may be taking
- Propylthiouracil (thyroid hormone antagonist, blocks synthesis of T3, T4 peripherally)
- Methimazole (thyroid hormone antagonist - inhibits synthesis of thyroid hormones by decreasing iodine use in the manufacture of thyroglobulin and iodothyronine)
- Potassium iodide (thyroid hormone antagonist, fosters colloid accumulation in thyroid follicles, decreases vascularity of gland)
- Glucocorticoids or Beta-blockers
Effects of Thyroid Hormones
Growth and maturation
- Skeletal muscle and CNS, required for normal mentation in adults (Cretinism)
- Enhances effects of catecholamines
- Increases HR
- Lipolysis
- Gluconeogenesis
- Generation of glucose from non-carbohydrate carbon substrates such as lactate, glycerol, and glucogenic amino acids
Basal metabolic rate (BMR)
- Oxidative metabolism, increased ATP production
- Thyroid hormone regulates basal metabolic rate
- Increased oxygen consumption - oxygen in phosphorylation (addition of a phosphate (PO4) group to a protein or other organic molecules) leading to an increase in heat
Carbohydrate, lipid, and protein metabolism
- Stimulates glycogenolysis and gluconeogenesis, lipogenesis and lipolysis, protein catabolism
> 99% of the hormone is bound to plasma proteins, providing a circulating reservoir
Preoperative Diagnosis
Definite/suspicious/inconclusive findings for malignancy, goiter, thyroid cancer (papillary, follicular, medullary, anaplastic (rare, 1%)), thyroid nodule, hyperthyroidism, Grave's disease
Hyperthyroidism
Elevated T3, T4, decreased TSH
Secondary to Graves' disease, toxic multinodular goiter, thyroid adenomas, TSH-secreting tumor (rare), or overdose of thyroid hormone
Symptoms
Fatigue, sweating, intolerance to heat
Increased appetite, weight loss, or gain
A-fib, palpitations are usually the first symptoms, CHF
Increased BP, HR, and pulse pressure
Increased thyroid levels
Thyroid goiter
Exophthalmos (antibodies to eye orbital muscles are common)
Nervousness, agitation
Thyroid Storm
Life-threatening exacerbation of hyperthyroidism during periods of stress. It can be mistaken intraoperatively for malignant hyperthermia, sepsis, anaphylaxis, and other hypermetabolic reactions
Symptoms
Hyperthermia >40 degrees C
Tachycardia
Widened pulse pressure
Anxiety
Altered mental status leading to psychosis, coma, and myopathy
Treatment
Increase FIO2
Fluid resuscitation
Electrolyte replacement/correction (increased Ca++)
Cooling blankets
Acetaminophen
Maintain diuresis
Treat precipitating events (infection, CHF, DKA, pregnancy)
Specific Treatment
Propylthiouracil (blocks synthesis)
- Block synthesis BEFORE giving iodides to block release
- Otherwise, "iodine escape" will occur later, and thyroid hormones will be produced
- 1 hr is adequate
Sodium Iodide (blocks release)
Steroids (unclear mechanism)
Beta-blockers (caution reactive airway, CHF)
Anesthetic Consideration
Ensure euthyroid state (check temp, HR, pulse pressure, and reflexes)
Supine position with extended neck and pillow under upper back to expose surgical site
Tracheal compression from large goiters can cause tracheal deviation, stridor
Increased basic metabolic rate causes increased Vo2 (oxygen uptake) and rapid desaturation on induction
Beta-blocker therapy for increased HR
Generous sedation due to nervousness
Avoid agents that stimulate the sympathetic nervous system
- Ketamine, pancuronium, meperidine
Visualize vocal cords function before extubation
The ability to phonate "e" post-extubation implies continued vocal cord function
Avoid coughing on emergence
Maintain normothermia
Emergence
There is an increased risk of airway obstruction after this procedure
- Secondary to recurrent laryngeal nerve damage
- Bilateral: the patient is unable to speak and requires reintubation
- Unilateral: hoarseness
Tracheomalacia (weakness and floppiness of tracheal cartilage) or hematoma
- Rapid intubation may be lifesaving if hematoma reopens the incision and drains blood
Acute hypoparathyroidism (hypocalcemia)
- It can present as a laryngeal stridor 24-48 hrs postop and may start with tingling of fingertips and lips, which, untreated, can progress to tetany and seizures
- Give 1 amp of Ca++ gluconate iv over 20 min will usually alleviate symptoms
Hypothyroidism
Decreased T3, T4, elevated TSH
Autoimmune disease destroys follicular epithelial cells. The patient cannot make thyroid hormone
Seen in elderly patients
Symptoms
Cold intolerance
- Depression of BMR
Decreased appetite and weight gain due to depression of BMR with low protein and fat metabolism
Decreased HR, pulse pressure
Edema (Myxedema)
- Accumulation of protein - mucopolysaccharides under the skin, water in interstitial space
Cretinism
- CNS development impaired
- Replace thyroid deficiency in the first few days to prevent long-term developmental side effects
Myxedema Coma
Severe hypothyroidism has mortality >50%
Symptoms
Stupor or coma
Hypothermia
Hypoventilation with hypoxemia
Bradycardia HR 50-60
Hypotension
Apathy
Hoarseness
Hyponatremia
Treatment
Early intubation
Treat low BP cautiously with volume, inotropes, pacing
Passive warming if temp >30C
Specific Treatment
L-Thyroxine (T4) or
Triiodothyronine (T3)
Hydrocortisone
Deceased TSH earliest sign of response to treatment
Anesthetic Considerations
Ensure euthyroid state
- Check temp, HR, pulse pressure, and reflexes
Supine position with extended neck and pillow under upper back to expose surgical site
Tracheal compression from large goiters can cause tracheal deviation, stridor
May see increased sensitivity to anesthetic agents and muscle relaxants
Decreased ventilatory response to increased CO2 and reduced O2
Bradydysrhythmias, diastolic HTN, decreased LV compliance, pericardial effusions
Addison's disease occurs in 5-10% - (no aldosterone, no cortisol) - may need steroids during surgery due to stress
Decreased basic metabolic rate, temperature
May have joint pain, myalgia
Anemia, GI bleeding, constipation, ileus
Visualize vocal cords function before extubation
The ability to phonate "e" post-extubation implies continued vocal cord function
Avoid coughing on emergence
Maintain normothermia
Emergence
There is an increased risk of airway obstruction after this procedure
- Secondary to recurrent laryngeal nerve damage
- Bilateral: the patient is unable to speak and requires reintubation
- Unilateral: hoarseness
Tracheomalacia (weakness and floppiness of tracheal cartilage) or hematoma
- Rapid intubation may be lifesaving if hematoma reopens the incision and drains blood
Acute hypoparathyroidism (hypocalcemia)
- It can present as a laryngeal stridor 24-48 hrs postop and may start with tingling of fingertips and lips, which, untreated, can progress to tetany and seizures
- Give 1 amp of Ca++ gluconate iv over 20 min will usually alleviate symptoms