A small compilation of nurse anesthesia care plans
These anesthesia care plans are meant to inspire nurse anesthesia residents when they are making their care plans. Always make sure you fully understand and "own" your care plan. Your plan must be specific for your patient and should always be with the most up-to-date information.
Tonsillectomy and Adenoidectomy
Etiology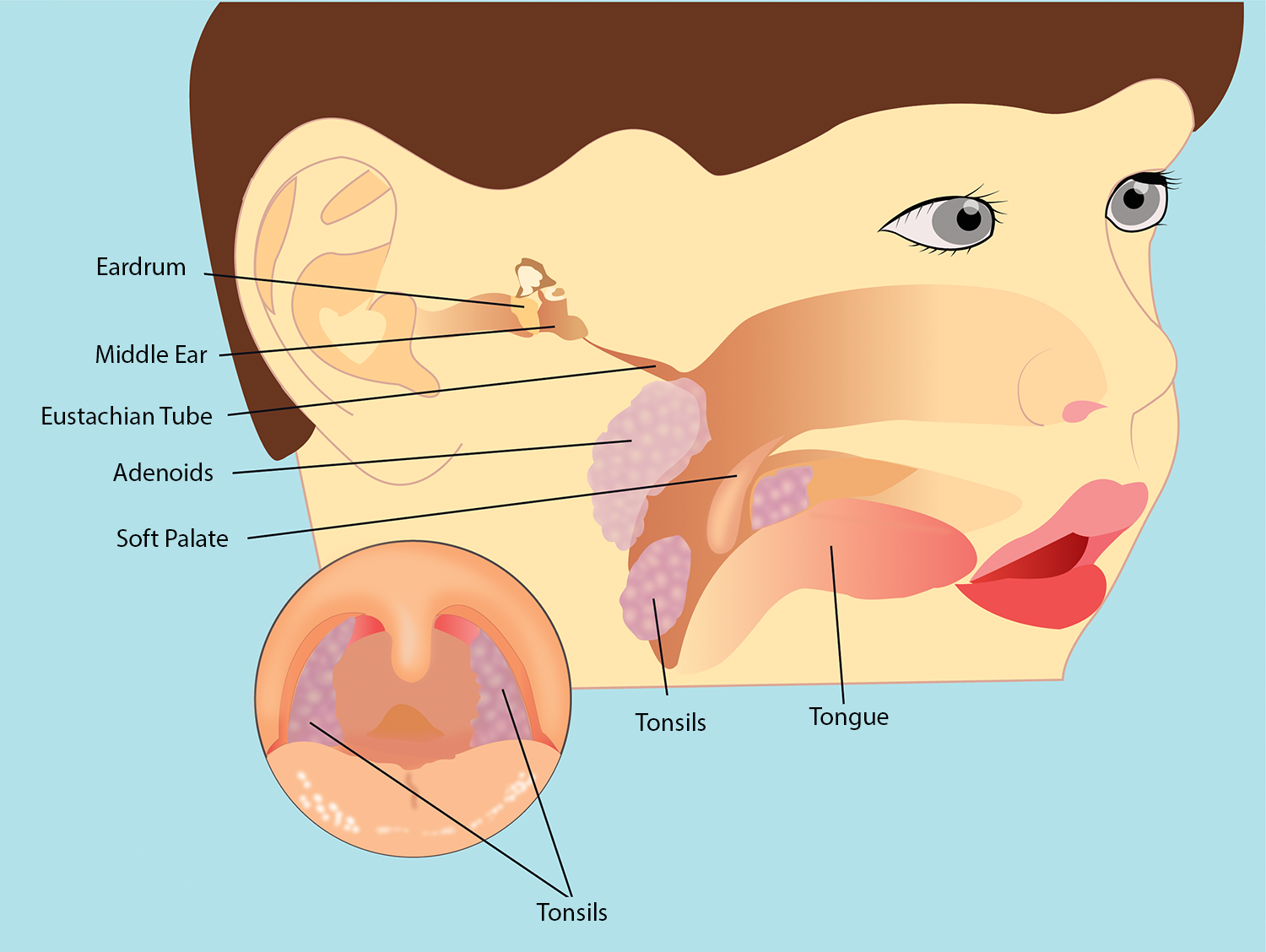
The cause of obstructive sleep apnea (OSA) in children is usually due to enlarged adenoid and tonsillar tissues. However, nasal obstruction due to enlarged turbinates and jaw deformity can also be major contributors to developing OSA.
- The primary treatment for OSA in children is adenoidectomy and tonsillectomy.
Children with OSA are at an increased risk for airway obstruction, respiratory distress, and the potential for apnea in the postoperative period.
Children hypoventilate and develop hypercarbia and arterial hypoxemia.
Preoperative Diagnosis
OSA, chronic tonsillitis and/or adenoiditis, tonsillar and adenoid hypertrophy, asymmetric enlargement of tonsils
Other symptoms are nasopharyngeal obstruction, obligatory mouth breathing, failure to thrive due to poor feeding, disturbances of speech and sleep
Chronic nasal obstruction may result in narrowing of the upper airway and dental and facial changes
May see airway obstruction, OSA, CO2 retention, and cor pulmonale
Sleep study
Apnea-hypopnea index - AHI (partial occlusion)
Pauses must be 10 seconds long to be significant; you might see a drop in O2 saturation
Respiratory disturbance index (RDI)
- AHI 5-15 mild, 15-30 moderate (daytime sleepiness), >30 severe (cardiac risk)
Preoperative considerations
Surgery
The patient is supine, shoulders slightly elevated on shoulder roll, and a mouth gag is inserted. Tonsils are removed, and hemostasis is obtained using packs and suction electrocautery
EBL
10 - 200 ml, monitor closely
Morbidity
Bleeding, aspiration, tooth damage
Pain Score
Adenoidectomy 3-5
Tonsillectomy 6-9
Age
2-8 yrs
Anesthetic Considerations
Monitor for any loose teeth. Advise parents that they may be dislodged with mouth gag/laryngoscopy manipulation
Oral airway to prevent airway obstruction on induction
An oral ray is placed midline to facilitate prompt placement of the mouth gag
- Cuffed to minimize drainage to the abdomen, recheck bilateral breath sounds
If the throat pack is in place - ensure removal prior to extubation
Monitor the airway closely with manipulation of the mouth gag
The neck may be extended - evaluate pt for any neck issues/atlantoaxial subluxation
Risk of airway fire - decrease FiO2 as tolerated, should be less than 30% for procedures above the nipple line
Risk of blood in the stomach - N/V
Suction midline only
Careful with opioid dosing due to OSA (increases risk of hypoventilation)
Extubate when fully awake
- There is a high risk of negative pulmonary edema due to previous obstruction to inhalations
- Pt might continue to inspire with force
May give Decadron
May give Zofran
Lateral position to PACU