A small compilation of nurse anesthesia care plans
These anesthesia care plans are meant to inspire nurse anesthesia residents when they are making their care plans. Always make sure you fully understand and "own" your care plan. Your plan must be specific for your patient and should always be with the most up-to-date information.
Transsphenoidal Surgery
Pituitary gland hormone production may be influenced by tumor location and/or hypersecretion caused by adenoma.
Anterior Pituitary
FSH/LH
May cause male impotence or secondary amenorrhea
Prolactin
Causes galactorrhea
ACTH
Excess production causes Cushing's disease (elevated cortisol levels)
Growth Hormone
Excess causes acromegaly (influences anesthesia as hypertrophy occurs in skeletal, connective, and soft tissues
The patient may have an enlarged tongue and epiglottis, making them prone to airway obstruction and possibly difficult intubation
- Have a glide scope in the room
Hoarseness may indicate thickening of vocal cords or issues with recurrent laryngeal nerve due to stretching
Dyspnea or stridor may indicate subglottic narrowing
Do a thorough airway assessment and consider awake intubation
The patient may also present with peripheral nerve injuries, HTN, or diabetes mellitus
TSH
Rarely excess production
Posterior Pituitary
ADH/Vasopressin
ADH as multiple functions
- Maintains extracellular fluid volume and regulates plasma osmolality
- Increases BP by constricting smooth vascular muscle (careful with cardiac disease pts, can cause ischemia)
- Promotes hemostasis through an increase in von Willebrand factor and factor VIII (accelerates coagulation)
The main stimulus is plasma osmolality, but also positive pressure ventilation, stress, anxiety, hyperthermia, B-adrenergic stimulation or histamine release can cause increased secretion of ADH
Diabetes Insipidus
Failure to secrete adequate ADH
- Results in significant increase in diuresis, hypernatremia (dehydration) and hypovolemia, poorly concentrated urine
Treatment
If complete DI, administer infusion of aqueous ADH 100-200mU/hr along with isotonic infusion while monitoring serum sodium and plasma osmolality
Pt may also receive ADH IM or DDAVP intranasally, which has prolonged action of 12 - 24hrs.
Excessive ADH Production
Caused by head injuries, intracranial tumors, pulmonary infections, small cell carcinoma of the lung, and hypothyroidism (causes hypothermia, which causes coagulopathy)
- Results in dilutional hyponatremia, decreased serum osmolality, decreased urine output with increased osmolality
- Weight gain, skeletal muscle weakness (low Na), mental confusion, or convulsions
Treatment
Fluid restriction, democlocycline, which interferes with the ability of the renal tubules to concentrate urine
Oxytocin
Contraction of the uterus stimulates milk production.
Transsphenoidal Resection Procedure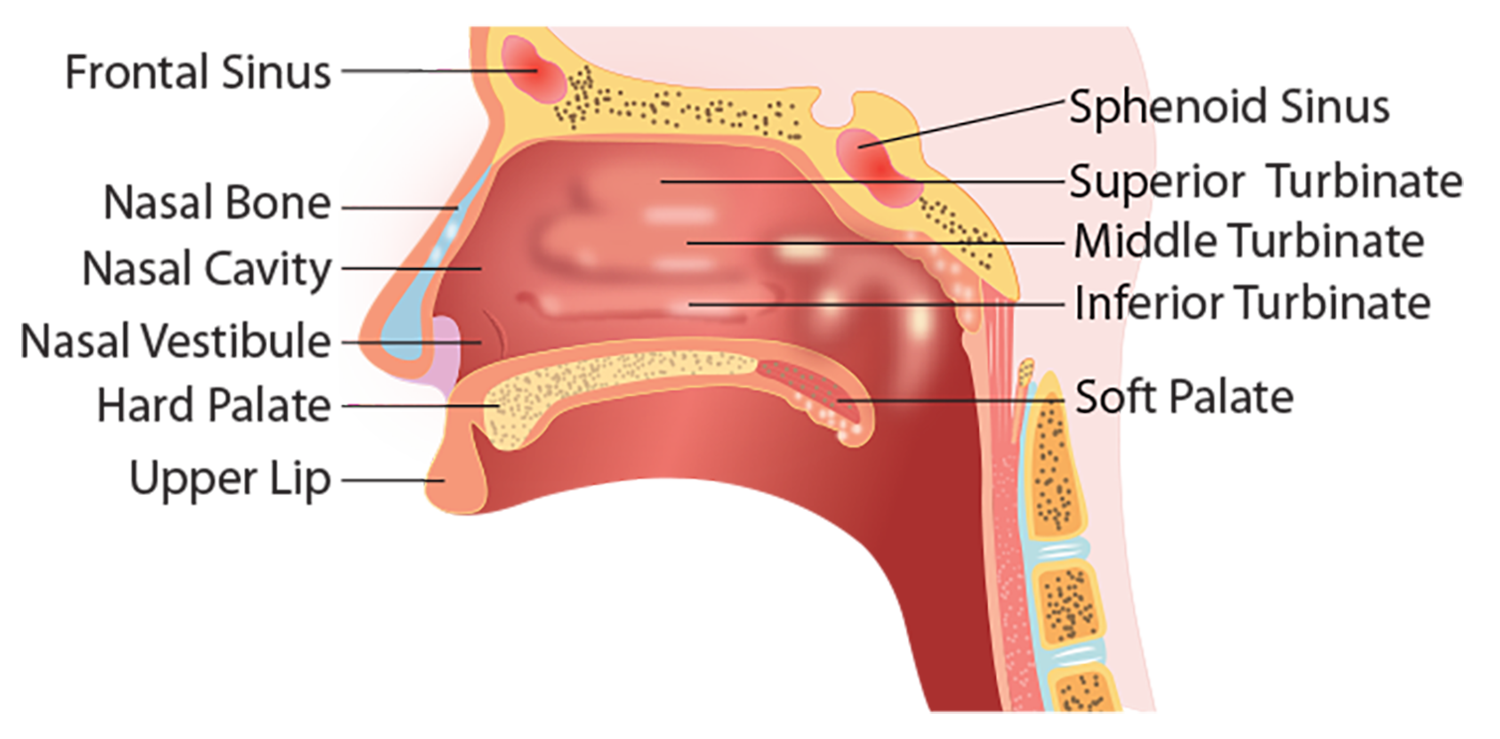
Presenting symptoms
- Hormone abnormalities, vision (usually loss of side vision, N/V, possible headaches
Tumors <10 mm usually via transsphenoidal approach, whereas tumors >20 mm via bifrontal craniotomy
The approach to sella turcica and region is associated with fewer complications than craniotomy
Access transnasally involves the creation of a tunnel to the sphenoid sinus. The sphenoid's rostrum (beak-like shape) is removed, the floor of the sella is removed, the Dura is opened, and the tumor is removed using microcurettes. Fat taken from the subcutaneous tissue at the time of the facial resection, or abdomen or thigh used to fill the sphenoid and hold the graft material in place (to seal the Dura if CSF leaks)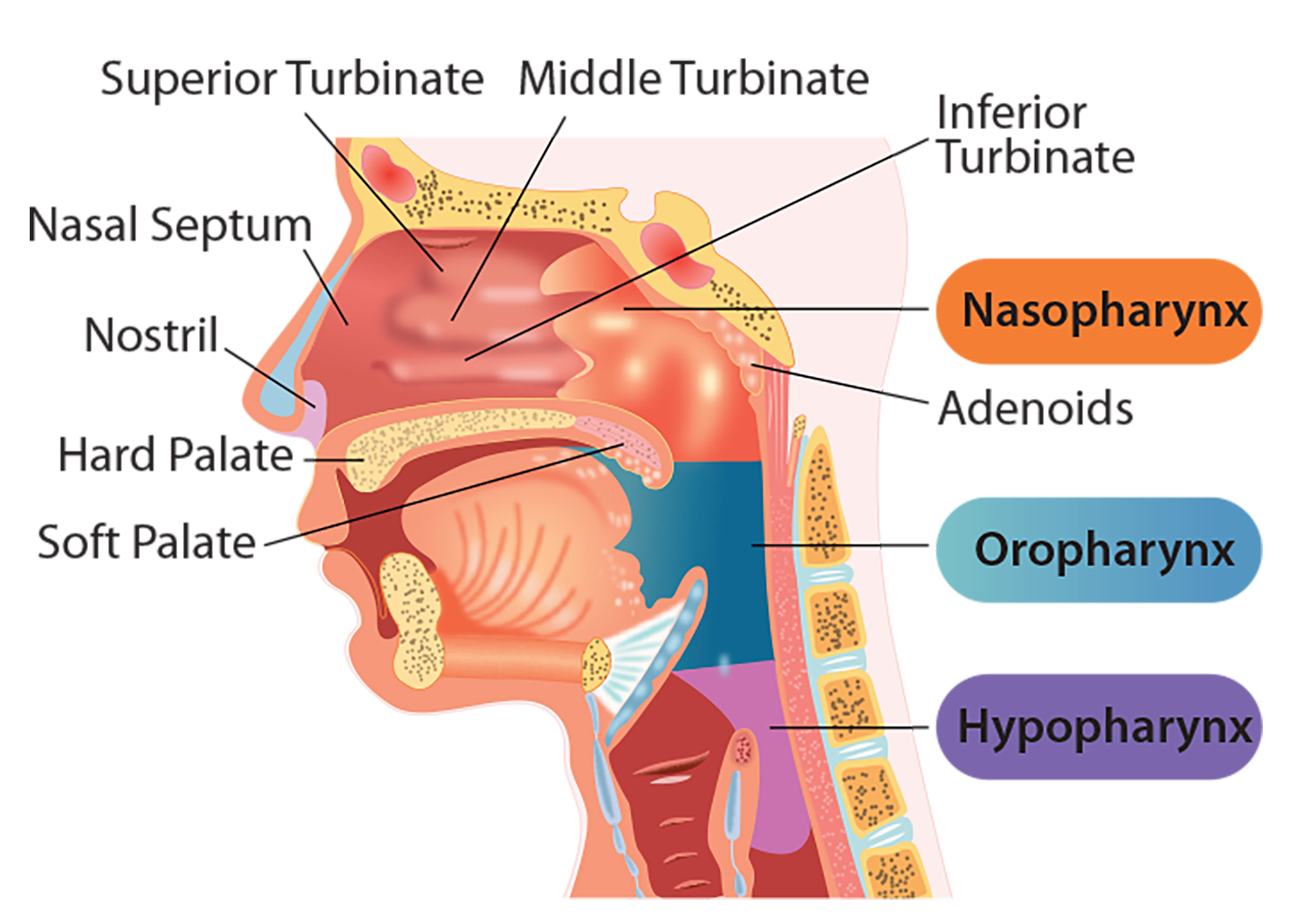
The lateral wall of the sphenoid sinus protects part of the optic nerve and the carotid artery
Operation is performed using a microscope and/or endoscope, mainly in the midline position, to protect the carotid arteries
The floor of the sella is reconstructed as needed, and the sphenoid bone may be packed and sealed like the Sella
The endoscopic approach provides improved surgical view and access, fewer complications, and faster recovery
Position
Supine, head elevated 20-30 degrees
Ensure 2-3 fingerbreadths between chin and chest
Possible Mayfield tongs placed by the surgeon to stabilize the head for seated access and to help with surgical drainage or a three-point pin head holder
- Premedicate with opioids before placement of Mayfield
- Very painful
The surgeon then correlates the CT/MRI findings with neurological marking, and you can retape the eyes afterward
Possible throat pack to prevent aspiration of blood
All pressure points are padded, and arms are tucked
Considerations
The possible use of evoked potentials influences the choice of anesthesia
ETT is taped out of the surgeon's way, and oral RAE is used. Secure well, as shared airway with the surgeon
Vasoconstrictors to the nasal area may cause elevated BP and dysrhythmia
Painful dissection of the nasal cavity can cause elevated BP and ICP
No hyperventilation as decreased ICP can lead to retraction of the pituitary gland = making it difficult to get to the surgical field
Risk of massive bleeding from carotid arteries
F/C to monitor urine output
The risk of post-op DI usually resolves in about 10 days
Avoid hyperglycemia (keep BS < 140-180)
Preoperative considerations
Antibiotics
Per surgeon
Surgical Time
2.5-3 hrs
EBL
25-250 mL
Age Range
18-85 yr (usually 30-50yr)
Mortality
1 %
Information
Patient ID, consent, NPO, HX, allergies, airway assessment. Questions answered. Premedicate with Versed and Robinul (consider the risk of increased ICP due to hypoventilation and subsequent elevated CO2)
Inform the patient of possible nasal packing post-op, so they will have to breathe through the mouth
Complications
Carotid artery injury (rare)
Venous air embolism
Hypopituitarism - note the need for steroid replacement (due to lack of cortisol)
Diabetes Insipidus 24-48 hrs postop
CSF leak
Epistaxis
Meningitis
SIADH
Cranial nerve injury
- Optical nerve with loss of vision
Anesthesia Considerations
Induction
GETA
May need lumbar drain if elevated ICP (tumors usually located in sella turcica and thus no elevation of ICP)
Oral RAE secured the left side of the mouth
OGT? to empty the stomach of blood post-op
Eyes taped and then protected with Tegaderm
- May wait to do final taping until the surgeon has done marking as mentioned above
Note surgical infiltration with epinephrine - monitor for dysrhythmia
Drugs to Consider
Lidocaine 1 mg/kg
Rocuronium: 5 mg pre-succinylcholine to prevent myalgias (10 mg/mL)
Propofol 1-2 mg/kg, possible infusion if doing TIVA
Succinylcholine 0.5-1.5 mg/kg (can cause elevated ICP)
Opioid
Fentanyl 1-3 mcg/kg IV
Remifentanil drip
Sufentanil - shorter duration of action and elimination half-life than fentanyl (high protein binding, low volume of distribution, tighter bound to receptors. Excreted via liver, little by renal)
Rule of thumb: Sufentanil is 10 times as potent as fentanyl
Maintenance
Consider modified hypotension to minimize bleeding along with the elevated head
O2/Isoflurane <1 MAC (must prevent vasodilation)
Fentanyl 1-10 mcg/kg or sufentanil 1-2 mcg/kg
Atracurium or vecuronium
Zofran 4 mg IV
Emergence
Reversal with neostigmine and glycopyrrolate or sugammadex
Lidocaine IV and via ETT to prevent any coughing
If coughing and not ready to extubate, give a little propofol IV
Extubate deep if possible. The patient must have spontaneous ventilation, been suctioned, and then emerge on a mask (this can also be difficult depending on the nasal status)
Remove tracheal packing if applicable